Millions of tubewells across the Indo-Gangetic plain supply drinking water that is relatively free of microbial contaminants. However, many of these tubewells tap groundwater that is high in arsenic and should be used only for washing. This column explores a new approach to field testing in order to distinguish safe from unsafe wells, and suggests that people are willing to pay for tubewell testing.
The number of tubewells installed in the soft sediments of the Indo-Gangetic plain and similar low-lying environments across South and Southeast Asia has grown exponentially over the past few decades. The boom was triggered by the availability of inexpensive PVC pipes and early installations supported by donors and non-governmental organisations (NGO) in order to reduce infant mortality. Most tubewells used today, however, were each commissioned privately by a few households pooling their resources to pay the equivalent of $50-150 for access to what was long held to be safe drinking water.
A large study conducted in Bangladesh has shown that drinking groundwater containing arsenic concentrations an order of magnitude higher than the current World Health Organization (WHO) guideline of 10 microgram per liter doubles all-cause deaths, primarily due to cardio-vascular disease (Argos et al. 2010, Chen et al., 2011). Arsenic in tubewell water has also been associated with increased infant mortality and impaired intellectual and motor function in children (Wasserman et al. 2004, Rahman et al. 2010, Parvez et al. 2011). Exposure to arsenic causes various cancers (Smith et al. 2000) and has been associated with a significant drop in household income in Bangladesh (Pitt et al. 2012).
Household responses to information
Much of the exposure to arsenic across South and Southeast Asia is avoidable. Several blanket surveys combined with more limited monitoring have demonstrated that the distribution of arsenic in groundwater is highly variable spatially, even with a single village, but typically stable through time. Within an area of Bangladesh where half of 5,000 tubewells are unsafe, almost 90% of households live within 100 meters of a safe well (van Geen et al. 2002). Spatial variability therefore makes it harder to distinguish safe and unsafe wells but also represents an opportunity for households to share the subset of safe wells.
In response to well testing, between one-third and two-thirds of households with an unsafe well have switched their consumption to a neighbouring well (Ahmed et al. 2006, Chen et al. 2007, Opar et al. 2007, Madajewizcz et al. 2007, Bennear et al. 2012, George et al. 2012a, Inauen et al. 2013). Switching between existing wells is therefore a promising option in the short term, while longer-term solutions continue to be investigated. Treating groundwater for arsenic at the household or village-level is a logistically much more complex option than testing and well-switching and, despite typically higher visibility in the development community and the media, has had little impact (Ahmed et al 2006).
The need for field-kit testing
The latest generation of field kits readily distinguishes the subset of wells within a village that can be used for drinking and cooking from those suitable only for washing (George et al. 2012b). Field-kit testing is vastly preferable to laboratory testing because the results can be communicated directly to the households.
The problem is that the drilling of new wells continues unabated and there currently is no financial incentive for testing new wells. Even in areas where a blanket survey has been conducted within the past decade, a majority of households do not know the status of their well because it has been installed more recently and never been tested (George et al. 2012a).
Testing for a fee
In a recent intervention in the state of Bihar supported by the International Growth Center (IGC), we explored a semi-commercial approach to testing that could potentially reduce the proportion of untested wells in use. Young graduates from a local university were trained to deploy the ITS Econo-Quick Arsenic kit (George et al. 2012b) and to enter data, along with additional well and household information, directly on a hand-held Global Positioning System (GPS) receiver. 26 small- to medium-sized villages within a 250 sq. km. arsenic-affected area south of the Ganges River were selected for the study. The villages were randomly divided in five groups where field testing was offered to individual households at prices of Rs. 10, 20, 30, 40, 50 / test (approximately $0.20-1/ test), respectively.
When reaching a village for the first time, testers displayed a billboard-sized map of that village generated in Google Earth to attract attention (Figure 1). A public-health message describing the risks of drinking high-arsenic groundwater was delivered and a second map showing the mixed distribution of arsenic in a neighbouring village was shown. The testers then announced that they were going to offer to test wells at a given price over the next several days by going door-to-door through the village. The testers also asked if there were any community wells associated with a school, temple, or mosque and typically tested those sources first.
Figure 1. Display of test results from neighboring village with a map produced in Google Earth
Test results were attached to each pumphead with a metal placard colored red (>50 ug/L arsenic), green (>10-50 ug/L), or blue (< 10 ug/L) to categorise wells relative to the national standard for arsenic at the time of 50 ug/L and the WHO guideline of 10 ug/L (Rajiv Gandhi National Rural Drinking Water Mission, Government of India has since matched its standard for arsenic in drinking water to the WHO guideline). After the testing was completed, a new Google Earth map showing the test results was posted at a central location in each village (the position of the wells was jittered by 20-40 m in order to limit the identification of specific households).
Figure 2 Metal placards with test results attached to pumphead

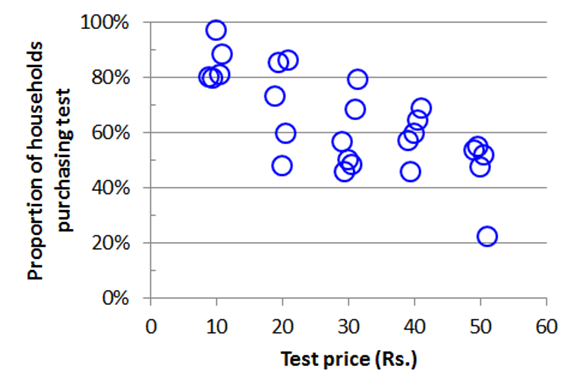
Of the 1,804 households that could be contacted, 1,195 agreed to have their well tested for a fee. Blue, green, and red placards were attached to 63%, 17%, and 20% of the tested wells respectively. Only 28 households claimed to know the status of their well even though this area has repeatedly been the subject of research and press coverage. When disaggregated to the village level, the data show that the proportion of households buying a test gradually declined as the price increased, even if this proportion also varied at any given price by +20% from one village to the other (Figure 3).
Figure 3 Relationship between demand for testing for each of the 26 villages and price charged
Implications for policy
This intervention demonstrated that there is a market to have tubewells tested for arsenic. The 20 Rs price that more than two-thirds of households in a village were willing to pay would be sufficient to cover the salary and transportation of a tester with secondary education, assuming 10-20 wells are tested in a day. However, the generated income would not be sufficient to cover the estimated total cost of testing when quality-control by a supervisor, a durable metal placard with the test result, kit supplies, and a GPS unit of 100-150 Rs/ test ($2-3) are included. These additional costs would therefore have to be covered centrally in future testing campaigns.
The State Health Society of Bihar has been contacted to discuss the possibility of a state-wide expansion of the tubewell testing campaign. Efforts to test millions of tubewells whose status is unknown should be initiated in other states of India and neighbouring countries affected by high arsenic levels in groundwater.
Watch a video of Chander Kumar Singh presenting the underlying research at the 2nd IGC South Asia Growth Conference (July 2013; New Delhi)
Further Reading
- Ahmed, M.F., S. Ahuja, M. Alauddin, S. J. Hug, J.R. Lloyd, A. Pfaff, T. Pichler, C. Saltikov, M. Stute, and A. van Geen, Ensuring safe drinking water in Bangladesh, Science 314, 1687-1688, 2006.
- Bennear L, A Tarozzi, A Pfaff, HB Soumya, KM Ahmed, A van Geen, Impacts of a randomized controlled trial in arsenic risk communication on household water supply choices in Bangladesh, Journal of Environmental Economics and Management, http://dx.doi.org/10.1016/j.jeem.2012.07.006, 2012.
- Chen, Y., A. van Geen , J. Graziano , A. Pfaff, M. Madajewicz, F. Parvez , I. Hussain, Z. Cheng, V. Slavkovich, T. Islam, and H. Ahsan, Reduction in urinary arsenic levels in response to arsenic mitigation in Araihazar, Bangladesh, Environmental Health Perspectives 115, 917-923, 2007.
- George CM, Graziano JH, Mey JL, van Geen A, Impact on arsenic exposure of a growing proportion of untested wells in Bangladesh, Environmental Health 11:7, DOI: 10.1186/1476-069X-11-7, 2012a.
- George, CM, Y Zheng, JH Graziano, SB Rasul, JL Mey, A van Geen, Evaluation of an arsenic test Kit for rapid well screening in Bangladesh, Environmental Science and Technology, accepted August 2012b.
- Inauen J, Hossain MM, Johnston RB, Mosler H-J, Acceptance and use of eight arsenic-safe drinking water options in Bangladesh. PLoS ONE 8(1): e53640. doi:10.1371/journal.pone.0053640, 2013.
- Madajewicz, M., A. Pfaff, A. van Geen, J. Graziano, I. Hussein, H. Momotaj, R. Sylvi, and H. Ahsan, Can information alone both improve awareness and change behavior? Response to arsenic contamination of groundwater in Bangladesh, Journal of Development Economics 84, 731–754, 2007.
- Opar, A., A. Pfaff, A. A. Seddique, K. M. Ahmed, J. H. Graziano, and A. van Geen, Responses of 6500 households to arsenic mitigation in Araihazar, Bangladesh, Health & Place 13, 164-172, 2007.
- Parvez F, GA Wasserman, P Factor-Litvak, X Liu, V Slavkovich, AB Siddique, Rebeka Sultana, Ruksana Sultana, T Islam, D Levy, JL Mey, A van Geen, KM Khan, J Kline, H Ahsan, JH Graziano, Arsenic exposure and motor function among children in Bangladesh, Environmental Health Perspectives 119:1665-1670, 2011.
- Pitt, M, MR Rosenzweig, N Hassan, Identifying the hidden costs of a public health success: Arsenic well water contamination and productivity in Bangladesh, PSTC Working Paper Series 2012-02. http://brown.edu/academics/population-studies/sites/brown.edu.academics.population-studies/files/uploads/2012-02-PSTC-Working-Paper.pdf
- Rahman A, LA Persson, B Nermell, SE Arifeen, EC Ekstrom, AH Smith, M Vahter, Arsenic exposure and risk of spontaneous abortion, stillbirth, and infant mortality, Epidemiology 21, 797–804, 2010.
- Smith AH, EO Lingas, M Rahman, Contamination of drinking-water by arsenic in Bangladesh: a public health emergency, Bulletin of the World Health Organization 78, 1093-1103, 2000.
- Wasserman, G.A., X. Liu, F. Parvez, H. Ahsan, P. Factor-Litvak, A. van Geen, Z. Cheng, V. Slavkovich, I. Hussain, H. Momotaj, J. H. Graziano, Water arsenic exposure and children’s intellectual function in Araihazar, Bangladesh, Environmental Health Perspectives 112, 1329-1333, 2004.




 11 March, 2013
11 March, 2013 




Comments will be held for moderation. Your contact information will not be made public.