To address absenteeism among staff at public healthcare facilities, the government of Karnataka introduced an innovative biometric device to monitor and enforce attendance rules. This column presents findings of a large randomised evaluation of the programme. While some health gains were achieved, imperfect enforcement illustrates the limits of monitoring solutions if there are constraints on full implementation in practice.
Needing to see a doctor or nurse, only to find them absent from work is frustrating. But, more than that, it can have serious consequences on public health. If the clinic is always closed, why make the effort to go and get primary care? Why should pregnant women seek antenatal care or plan to deliver in an institution if they do not trust health professionals to be present? In the long-run, high absenteeism can dissuade citizens from accessing healthcare at public facilities, perhaps leading them to visit untrained or unqualified providers for treatment.
While it seems crazy to think that someone would just not show up for their job, this is sadly the reality of the public health system in many rural Indian towns. In our baseline data for five districts in Karnataka, doctors were only present during their required hours 40% of the time. Nurses - only 49% of the time. In the most rural district that we studied, doctors were only present 15% of the time.
What drives this high rate of absence?
Health staff in Karnataka mentioned how far the public clinics were from their homes, and the lack of reliable and frequent public transportation. They also cited 'field' duties and meetings, as well as frustration at the lack of appreciation for their services. On the other hand, government officials and citizens suggested that private practices doctors run on the side, coupled with the challenges of monitoring health staff, were to blame.
What can be done to combat the absence? This is the question the National Rural Health Mission (NRHM) of the state of Karnataka aimed to answer.
A research-policy partnership to advance a state initiative
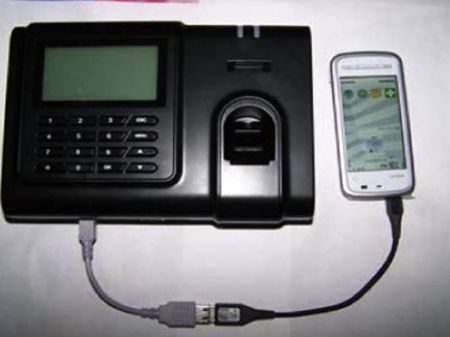
In 2010, the NRHM decided to pilot a programme called the 'Integrated Medical Information and Disease Surveillance System (IMIDSS)'. The idea of the programme was to use biometric devices (connected to a mobile phone) to enforce the government's actual attendance rules.
We collaborated with the government to design and run a randomised evaluation to study the impacts of IMIDSS on attendance and ultimately health. We randomised the IMIDSS in 140 of the 322 primary health centres (PHCs) that existed in five districts - Mysore, Chitradurga, Dharwad, Dakshina Kannada, and Bidar - that were chosen as they are representative of the socioeconomic and administrative diversity of the state. Even as a pilot, this was a massive undertaking with the potential to impact the attendance of hundreds of government employees and the healthcare of 2.5 million citizens.
Prior to the introduction of the IMIDSS, PHC staff recorded attendance on paper registers that are monitored by the doctors. The staff generally have 15 days of 'casual' leave that must be used within the calendar year or they lose it, and they can also accumulate up to 30 days of 'earned leave'. This earned leave is valuable because a large part of it can be cashed out, either during the year or at retirement, creating incentives to be absent without registering a leave.
While 182 comparison PHCs continued to use paper registers, the 140 PHCs in the treatment group were equipped with an IMIDSS device, consisting of a fingerprint reader and a multipurpose mobile phone. The device was used to record staff attendance via thumb impression at the beginning and end of each day. Attendance data could be transferred wirelessly using the existing cellular network to the state health headquarters so supervisors could track attendance in near real-time. This data was analysed and then communicated back to the districts. Using the data, the government planned to issue both positive incentives, such as rewards for staff members with good attendance records, as well as negative incentives, such as reprimand letters, disciplinary action, docking of pay, and deduction of earned leave for employees with unauthorised absences.
The IMIDSS programme was implemented by the government and funded by the World Bank, while the field evaluation was implemented by the Abdul Latif Jameel Poverty Action Lab (J-PAL) South Asia and funded by J-PAL and USAID's (United States Agency for International Development) Development Innovations Venture (DIV). We conducted a baseline survey in July 2010 and seven rounds of post-programme attendance-monitoring surveys. In addition, we also conducted endline surveys with the various stakeholders (facility survey, doctors, nurses, sub-district health officials, local elected officials, citizens) to assess the programme impacts.
Did attendance increase?
Seeing the programme in action, our prior was that the IMIDSS would not be successful in reducing absence. This is because there were many delays in the government's rollout of the system and training of the health staff was generally weak. But, most importantly, while some 'show-cause' notices were sent, generally no staff members either received a penalty or deduction of their earned leave for being absent. Neither did anyone receive any rewards for good attendance. However, despite this attendance increased: overall attendance by healthcare staff increased by almost 9%, from a base of roughly 40% in the comparison group. But, all of this increase was due to nurses, lab technicians and pharmacists coming more, nearly 18% more. And, rather than this being an increase of days in the office, much of this was the health staff staying for a longer work day, rather than coming a few hours late. There was no change in the attendance of the doctors.
Were there changes in health behaviours and outcomes?
Would this change in absenteeism affect health-seeking behaviour or outcomes? It is not entirely clear - perhaps it is not a large enough increase to matter, or just having a nurse there, rather than the doctor, will not improve health. To better understand this question, we conducted a survey of women who gave birth during the project period, to learn more about health patterns across the treatment and comparison groups.
Health did improve: there was a 4.6 percentage point decrease in the probability of being born below 2,500 grams. Many women were already getting antenatal care, and this did not change as a result of the programme - thus, the gain in birth weight was not due to an increase in antenatal care seeking. However, one possible explanation for these results is that having the nurse and other health staff spend more hours at the PHC lead to more healthful visits. For example, we observe that the treatment women were much more likely to get iron folic acid tablets from the PHC relative to the comparison group.
One large change that the IMIDSS programme generated was a change in delivery methods: deliveries conducted by doctors increased by about 16% for women who lived near the treatment PHCs. Why would this occur, especially since doctor attendance did not change? This could be due to a number of factors: "delivery location also changed, with more women in the treatment areas delivering in the large public and private hospitals. Some of this may have been due to better triage by the more present nurses and pharmacists, sending women with high-risk pregnancies to the more advanced hospitals. Moreover, the women who had just delivered in the catchment area of the treatment PHCs were less satisfied with staff attendance at the treatment PHCs, so it is also possible that the treatment simply increased the salience of the absenteeism when the women came in for their antenatal visits."
Why withhold penalties?
Given the high level of absenteeism, the potential of the attendance monitoring system to affect health, and the cost savings that the government could achieve by not paying out earned leave for absent staff, why didn't the government better enforce the system? Why didn't the government penalise the staff?
At the top, despite good intentions, the state government officials, who conceived the project did not anticipate just how difficult it would be to act on the monitoring data; the process of deducting leave days is actually quite complex and requires cooperation among different government stakeholders; thus, in practice these deductions rarely ever occurred.
The reluctance to take action against absent doctors also reflected the government's overall challenges and tradeoffs in running a public healthcare system. Doctor vacancies are widespread as it is tough recruiting doctors to work in rural health centres, especially given the demand for doctors in the private sector in urban areas. Therefore, the government officials stated that they were reluctant to place too many expectations on the staff, particularly the doctors, in order to provide more flexible work schedules for them.
But, this study should serve a cautionary tale: one cannot simply drop in a new technology without being aware of the broader economic and political forces at play. It is important to understand how the system as a whole works, and pay attention to the human factor in the policy design.




 09 December, 2016
09 December, 2016 







Comments will be held for moderation. Your contact information will not be made public.