India’s 10-week long national lockdown to contain the spread of Covid-19 was among the most severe in the world. This article investigates the effects of the lockdown restrictions on healthcare access and health outcomes for patients needing life-saving chronic care. It finds that access to health services was severely disrupted; mortality increased by 64% between March and May 2020; and there was 25% total excess mortality in the four months after imposition of the lockdown.
On 24 March 2020, India announced a nationwide lockdown that barred people from leaving their homes, required non-essential commercial establishments and transport services to close, and was enforced strictly with penalty of arrest. Google Mobility data show that mobility decreased by 60-80% within days of the announcement. Although critical health services were officially exempt from the lockdown, widespread disruptions to routine and emergency non-Covid services have been documented (Smith et al. 2020, Prasad et al. 2020, IndiaSpend, 2020). However, quantifying the impact of these disruptions on health outcomes has remained difficult due to the unavailability of reliable and high-frequency data on morbidity and mortality. In the absence of administrative data, evaluating the effect of the Covid-19 lockdown on non-elective health services requires the identification of patients in need of such care and the collection of primary data.
In a new research study (Jain and Dupas 2020), we use insurance claims filed under a large-scale government health insurance programme in Rajasthan, to identify all patients requiring critical, chronic non-Covid healthcare. We focus on dialysis, a form of life-sustaining long-term hospital care that is typically required 2-4 times each week for the duration of the patient’s life. Missing dialysis visits or shortening their duration is associated with large increases in hospitalisation and mortality (Saran et al. 2003). We conducted a series of rapid phone surveys with the households of the identified patients between May and August 2020 to measure the effects of the lockdown on healthcare, morbidity, and mortality in the four months following its imposition.
Patients faced substantial disruptions to their care
Over 62% of patients report a disruption in access to dialysis care due to the lockdown (Figure 1). Travel barriers were the most common cause of disruptions. Interviews suggest that difficulties finding transport and requirements to show proof of official approval of travel exemptions for hospital visits, were contributing factors. Patients also faced hospital closures, service refusals, and increased charges. Twenty three per cent of patients had to switch to a different hospital from the one they typically visit. Although the lockdown was universal, its effects on care access were worse for lower-caste and poorer patients and those living further away from a hospital. Structured interviews with hospitals confirm patient reports, but also suggest that hospitals faced their own constraints – most hospitals reported large decreases in patient volumes due to travel barriers, and many had to close down due to staffing and supply shortages.
Figure 1. Disruptions to dialysis care during the Covid-19 lockdown
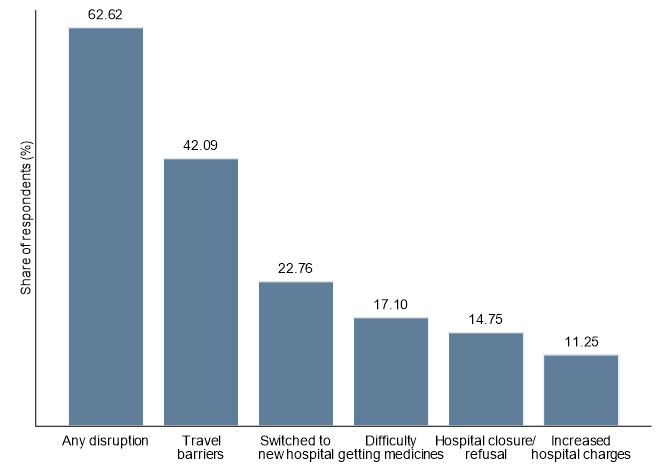
Note: The figure presents the share of patients that reported experiencing disruptions to their dialysis care due to the lockdown at any point between imposition of the lockdown and the first survey conducted during May-June 2020.
Below is an excerpt from an interview with the family member of a patient who died soon after the lockdown: “We live in [District A] and the hospital he regularly visited was in [District B]. When the lockdown was imposed and there was a curfew, he had to find a smaller, alternative facility for dialysis. We were asked to get permissions and multiple slips from government officials. He didn't get the care he usually received. That smaller hospital didn't do his dialysis properly and that's why he died. […] The medicines that were prescribed to him were only available in [District B] and not his local area due to the lockdown. He missed his medicines for BP and diabetes for 20 days.”
Mortality increased sharply in May, particularly among females and disadvantaged groups
To study changes in mortality, we plot the monthly mortality hazard, or the share of people alive that die in a month, over the four months before and after the lockdown. To examine whether monthly or seasonal fluctuations may explain any changes in mortality, we compare mortality in our survey sample with mortality in a similar cohort of patients in the previous year. Mortality declines steadily between December and March in both cohorts. This is expected, as the sickest and most vulnerable patients die early on at higher rates. However, between March and May 2020 (after a month of exposure to the lockdown), this trend reverses and mortality increases by 64%. Mortality in the previous year shows no such increase. Overall, comparing observed mortality during April-July 2020 to mortality in March 2020, and to mortality during April-July 2019, we estimate 22-25% total excess mortality in the four months after the lockdown.
Figure 2. Monthly mortality among dialysis patients
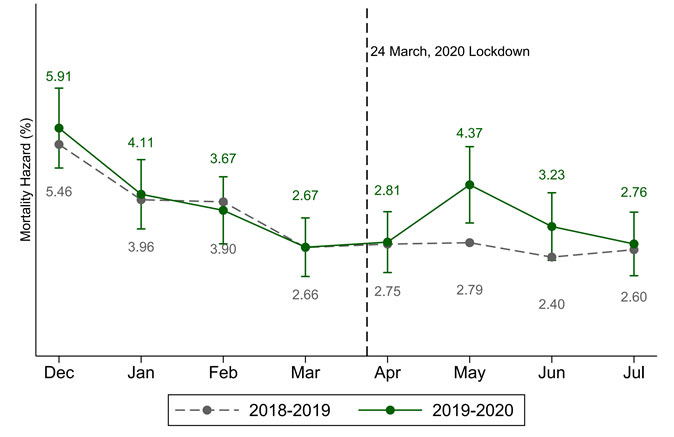
Notes: The figure presents the monthly mortality hazard (the share of people alive up to a month that die that month) among dialysis patients between December 2019 and July 2020 (solid green line) and for a comparable cohort of patients over the same months in the previous year (dashed grey line). While mortality declines steadily between December and March in both cohorts, it increases sharply from 2.67% in March to 4.37% in May (64% jump), and 3.23% in June 2020. Overall, the death rate during April-July 2020 was 22% higher than in March 2020, and 25% higher than in the same months in 2019.
This excess mortality is unlikely to be due to Covid-19 infections – only four patients in the sample were reported positive, and we find the largest increase in mortality in May, soon after the lockdown, whereas virus spread increased over time. Instead, we find evidence that excess mortality is driven by lockdown-related disruptions to dialysis care. Restricting the sample to patients alive at the end of April and exposed to at least one month of the lockdown, we find that an index of care disruptions is strongly associated with increased morbidity, hospitalisation, and death.
Analysis of variation in mortality by subgroup indicates that, while almost every subgroup experienced a large increase in mortality in May relative to March, the increase is larger for females and socioeconomically disadvantaged groups. Poor and lower-caste patients faced greater disruptions to their care, which may explain their higher mortality. The higher mortality among females than males, however, is not driven by females experiencing greater disruptions. Instead, we find some evidence that it may be due to lower care-seeking by households for females when they got sicker. While disruptions led to increased morbidity among both females and males, hospitalisations only increased for males, and mortality increased substantially more among females.
Discussion and policy implications
The timing and size of the mortality increase relative to pre-lockdown trends in 2020, as well as to trends in the previous year, strongly suggest that the observed increase is due to the nationwide Covid-19 lockdown. The fact that lockdown-related disruptions to dialysis care are positively associated with morbidity and mortality in subsequent months, provides further support for this interpretation. While our analysis is restricted to one type of care in one state, our findings are indicative of the serious but largely undocumented health effects of severe disruptions to similar critical health services across India. The national Pradhan Mantri Jan Arogya Yojana (PMJAY)1 health insurance programme saw a 6% reduction in dialysis claims, very similar to our results, a 64% decline in oncology care, and an 80% decrease in critical cardiovascular surgeries (Smith et al. 2020).
These findings highlight the unintended consequences of the lockdown on critical non-Covid health services that must be taken into account in the implementation of future policy efforts to control the spread of pandemics. Although critical health services were officially exempt from the lockdown, these were hard to implement in practice – patients had difficulties obtaining administrative exemptions and finding transport, and hospital and pharmacy supply chains were disrupted. Ensuring critical, non-elective health services continue uninterrupted through lockdown periods requires substantial prior administrative and health system planning. Furthermore, our finding that a universal policy had larger adverse effects on already vulnerable subpopulations (patients of low socioeconomic status, and those further away from the health system) indicates that these groups may require extra, targeted protections. We also find evidence that service access was not back to normal as of August, well after the lockdown was eased, suggesting that adverse effects on morbidity and mortality may continue to unfold over the coming months if further action is not taken.
Note:
- PMJAY is one of the two components of the Ayushman Bharat Yojana (National Health Protection Mission), which was launched in 2018. PMJAY is a health insurance programme that aims to reduce the financial burden on poor and vulnerable groups, arising out of catastrophic hospitalisation episodes.
Further Reading
- Jain, R and P Dupas (2020), ‘The Effects of India’s COVID-19 Lockdown on Critical Non-COVID Health Care and Outcomes’, Working Paper.
- Prasad, Narayan, Mansi Bhatt, Sanjay K Agarwal, HS Kohli, N Gopalakrishnan, Edwin Fernando, Manisha Sahay, Mohan Rajapurkar, Arpita Roy Chowdhary, Manish Rathi, Tarun Jeloka Valentine Lobo, Shivendra Singh, AK Bhalla, Umesh Khanna, SB Bansal, PK Rai, Amol Bhawane, Urmila Anandh, Ajit Kumar Singh, Bharat Shah, Amit Gupta and Vivekanand Jha (2020), “The adverse effect of COVID pandemic on the care of patients with kidney diseases in India”, Kidney International Reports, 5:1545-1550.
- Rukmini, S (2020), ‘COVID-19 disrupted India’s routine health services’, IndiaSpend, 27 August 2020.
- Saran, Rajiv, Jennifer Bragg-Gresham, Hugh C Rayner, David A Goodkin, Marcia L Keen, Paul C Van Dijk, Kiyoshi Kurokawa, Luis Piera, Akira Saito, Shunichi Fukuhara, Eric W Young, Philip J Held, Friedrich K Port (2003), “Nonadherence in hemodialysis: associations with mortality, hospitalization, and practice patterns in the DOPPS”, Kidney International, 64(1):254-262.
- Smith, O, P Naib, P Sehgal and S Chhabra (2020), ‘PM-JAY Under Lockdown: Evidence on Utilization Trends’, PM-JAY Policy Brief 8, National Health Authority.




 01 October, 2020
01 October, 2020 





Comments will be held for moderation. Your contact information will not be made public.