Debraj Ray and S Subramanian contend that despite the apparent sentiment of ‘we are all in this together’, the global burdens of Covid-19 and the global benefits of anti-Covid-19 policy have been skewed against the poorer nations of the world, and within nations, against the poor and the vulnerable.
It is no exaggeration to observe that the Covid-19 pandemic has been the single most newsworthy event of 2020, in a way and on a scale that has not been rivalled, over decades, by any other comparably unique phenomenon. We intend this as a purely positive statement – a simple search of Google Trends will readily confirm it – but when juxtaposed with other relatively neglected observations, it has practical and normative implications that deserve our attention.
Among these facts is the mortality caused by diseases other than Covid-19, the distribution of disease mortality across countries according to their economic standing, and the prioritisation of disease concerns that is reflected in the global consciousness of the issue, at both international and national levels. Among the consequences of the overwhelming preoccupation with Covid-19 is one aspect of the global response to it, namely, the stringent counter measures (such as a comprehensive lockdown) that poorer countries have had to go along with, for reasons that owe something both to the threat of the stick and the blandishment of the carrot. These issues form the subject matter of this post.
Global salience of Covid-19
On 11 March 2020, Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization (WHO), declared Covid-19 to be a pandemic, and the perceived global significance of the disease was underlined in no uncertain terms (WHO, 2020a): “WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction. We have therefore made the assessment that COVID-19 can be characterised as a pandemic. Pandemic is not a word to use lightly or carelessly. It is a word that, if misused, can cause unreasonable fear, or unjustified acceptance that the fight is over, leading to unnecessary suffering and death.”
In the months following this announcement, the pandemic received unrelenting attention in the news media, in social media outlets, and in academic work by practitioners associated with both the medical and the social sciences. The explosion on news and social media platforms has been quite accurately described as an “infodemic”, and the standard epidemiological model has even been applied to it, yielding enormous reproduction rates (or R0) for information dissemination on Twitter, Instagram, and the like (Cinelli et al. 2020).
In parallel vein, the scale of scientific work on Covid-19 has been massive. The WHO maintains a Global Covid-19 Database of research papers on the subject. The count, as of 16 February 2021, was a staggering 204,976. Nor is the WHO the only resource.1
Avinash Dixit’s tongue-in-cheek assessment of R0 for academic research on Covid-19 (Dixit 2020) also yields, not unexpectedly, large values for contagion, and he concludes with light-hearted policies for controlling the research epidemic, such as peer review as practised in economics: “Peer review can also delay the chain of infection. Economics has perfected this art; peer review in that field can stretch out over three or four years.” If only it were that easy to control the grim spread of the Virus instead!
Similarly, unprecedented has been the intensity of country-wise monitoring and tracking of the disease by data agencies on a daily basis – of mortality, infection, testing, and the stringency of government response. Some of the major data websites are the WHO’s COVID-19 Dashboard, Our World in Data, Statista, Worldometers, Covid19india.org, and The Oxford COVID-19 Government Response Tracker (OxCGRT). These responses have been strong enough that the United Nations has even warned of the attendant dangers of intrusive surveillance of citizens by government agencies (United Nations General Assembly, 2020).
All things considered, the global salience of Covid-19 has indeed been overwhelming. It is safe to say that no such comparable attention has been paid to other communicable diseases. Where do those diseases stand in relation to Covid-19?
Communicable diseases in richer and poorer countries
The WHO (2020b) classifies the top-10 causes of global mortality into three major categories: communicable, non-communicable (chronic), and injuries. The total death count for 2019 from these top-10 causes was estimated at 55.4 million. Our concern here is with the category of communicable diseases. Information on the 10 leading causes of death is available for each of four country-groupings based on the World Bank’s categorisation by per capita gross national income: low-income countries, lower middle-income countries, upper middle-income countries, and high-income countries.
There are four communicable diseases that appear in the infamous top-10 list in at least one of these four groupings. These are lower respiratory infections, neonatal conditions, diarrhoeal diseases, and tuberculosis (TB), which together we shall call ‘the four communicable diseases’ (or the 4C diseases, for short). Together, these accounted for 7.9 million of the global count of 55.4 million deaths in 2019. For reference, it should be noted that the global death count for Covid-19 for 2020 was around 1.8 million. Table 1 contains these aggregate statistics and some less aggregated information, to which we now turn.
For ease of exposition, we coarsen the World Bank’s four-fold classification into a binary one, consisting of one group we call the set of (relatively) ‘poorer countries’ (obtained by combining the low- and lower middle-income countries into a single category), and a second group we call the set of (relatively) ‘richer countries’ (obtained by merging the higher middle- and high-income countries).
Table 1. Global distribution of five major communicable diseases between poor and rich countries: 2019 and 2020
|
Disease |
Total deaths (m) |
Rich share (%) |
Deaths/million |
Ratio |
|||
|
All |
Rich |
Poor |
Rich |
Poor |
Poor/rich |
||
|
The 4C diseases |
7.91 |
2.08 |
5.83 |
26.30 |
508.3 |
1,627.7 |
3.20 |
|
Lower respiratory infections |
2.60 |
1.05 |
1.55 |
40.39 |
256.6 |
432.7 |
1.69 |
|
Neonatal conditions |
2.40 |
0.56 |
1.84 |
2.33 |
136.9 |
513.7 |
3.75 |
|
Diarrhoeal diseases |
1.51 |
0.11 |
1.40 |
7.29 |
26.9 |
390.9 |
14.53 |
|
Tuberculosis |
1.40 |
0.36 |
1.04 |
25.71 |
88.0 |
290.4 |
3.30 |
|
Covid-19 |
1.81 |
1.41 |
0.40 |
77.90 |
339.0 |
109.9 |
0.33 |
Notes: i) Data for Covid-19 pertain to 2020, and for other diseases to 2019. Mortality figures for the 4C diseases are from WHO. ii) Mortality figures for Covid-19 are from country-level data in Our World in Data and terminate on either 30 December or 31 December 2020. iii) Data are aggregated separately for richer and poorer countries, employing the World Bank's country groupings. iv) Country and world population figures for 2019 are from the World Bank, and global population figures for 2020 are from the Population Reference Bureau, 10 July 2020. v) Country population shares in 2020 are assumed to be the same in 2019.
Table 1 constructs a picture of the global distribution of deaths due to the 4C diseases in 2019, and the global distribution of deaths owing to Covid-19 in 2020, across poorer and richer countries.2 We do this by using both absolute mortality numbers (in millions) in the first three numerical columns and mortality per million in columns 5 and 6.3 The numbers are largely self-explanatory and do not require much elaboration. What we do wish to draw attention to is the significant asymmetry across richer and poorer countries.
Because poorer countries are still in the earlier stages of the epidemiological transition, deaths from contagious diseases are relatively high. The contrasts are dramatically depicted in Table 1 from various angles. Richer countries account for just 26.3% of all deaths from 4C diseases. That contrast is slightly heightened as we move to the per capita viewpoint highlighted in the later columns of Table 1, because richer countries have a somewhat larger population – approximately 4.1 billion compared to the roughly 3.6 billion in poorer countries4. The per capita mortality ratio from 4C diseases across poorer and richer countries is 3.2. If you live in a richer country, you are about 1.5 times as likely to die from a 4C disease as from Covid-19. But you are 15 times as likely to die from a 4C disease relative to Covid-19 if you are from a poorer country.
The contrast is particularly well-marked in the case of diarrhoeal diseases (where the per capita mortality ratio stands at over 14.5), somewhat less evident for lower respiratory infections (with a ratio of ‘just’ 1.7), and is typified by the differential mortality from TB (with a ratio of 3.3). All this is to be compared to the ratio of 0.33 from Covid-19.
In this context, two additional features of Covid-19 are worth taking note of. First, the 2020 Covid-19 global mortality figure is actually smaller than each of the corresponding figures for neonatal conditions and lower respiratory infections, while TB, with the lowest aggregate mortality count of 1.4 million, nevertheless registers a magnitude that is a substantial 78% of the magnitude of Covid-19 mortality. (And TB has taken its toll year after year – to a greater absolute degree in the past decades and certainly so as a fraction of world population for many more years.)
Yet, richer countries accounted for over three-quarters of the global Covid-19 mortality in 2020. That is to say, Covid-19 is by no means the single-most-deadly communicable disease in the world but it is the only one which, in terms of aggregate and per capita mortality, is decidedly more significant for richer countries than it is for poorer countries.
The differential implications of communicable diseases for the rich and the poor are fundamentally mediated by their mode of communication. For lower respiratory infections, the Centers for Disease Control and Prevention says (undated), “Many of the germs that cause respiratory (breathing) diseases are spread by droplets that come from coughing and sneezing. These germs are usually spread from person to person when uninfected persons are in close contact with a sick person. Some people may become infected by touching something with these germs on it and then touching their mouth or nose. In general, the best way to help prevent spread of respiratory germs is to avoid contact with droplets of secretions of saliva, mucus and tears.”
The principal mode of transmission is through casual person-to-person contact. This is, of course, true of Covid-19 as well. With the other infectious diseases, however, transmission is also profoundly mediated by conditions of poverty and nutrition. For the class of diarrhoeal diseases, the WHO (2017) indicates that “infection is spread through contaminated food or drinking water, or from person to person as a result of poor hygiene”.
The same is true of neonatal infections transmitted from mother to child or via the environment, during or after childbirth. As pointed out in Johns Hopkins Medicine (undated), several of these conditions are caused by viruses, fungi, parasites, and bacteria, and infection can arise from exposure to contaminated soil, water, fruits, and vegetables. Typical neonatal conditions would include Group B streptococcal disease, listeriosis, E.coli infection, meningitis, sepsis, conjunctivitis, candidiasis, and other congenital infections.
Mannava et al. (2019) observe: “The importance of hygiene practices during childbirth and the postpartum period is well recognised…. Practices such as hand washing by birth attendants, clean birthing surfaces and clean cord cutting are associated with reductions in all-cause sepsis and tetanus neonatal mortality…. These essential practices require adequate water, sanitation and hygiene (WASH) services.”
The point is that for a subset of communicable diseases, communication is mediated by poverty, and an improvement in socioeconomic conditions (while no guarantee against bad hygiene) serves as significant insulation. When that is taken into account, a communicable disease like Covid-19 is of vastly greater significance for richer countries, just as it is for rich populations within poorer countries. Covid-19 is nowhere near as class-conscious as the other communicable diseases we have mentioned.
Would, or should, such a skewed salience distort the optimal behaviour of a globally concerned social planner? Or, neglecting the preoccupations of richer countries for the moment and asking the question from a narrower and more self-interested perspective, should poorer countries buy into draconian measures to combat Covid-19 at the possible risk of neglecting other infectious diseases that ravage these societies? Of course, it is easy enough to insist that nothing should be neglected. But nothing comes for free and hard choices must be made.
The case of tuberculosis
Perhaps the sharpest expression of the divide between poorer and richer countries is to be found in a comparison of TB and Covid-19. TB is a bacterial disease, infectious just as Covid-19 is infectious. In 2019, an estimated 1.3-1.5 million individuals died of TB worldwide, with an overall global incidence just shy of 10 million.
A crude calculation of the case fatality rate (CFR) works out to 14%, which pools a large heterogeneity of cases (treated versus untreated, different strains of TB, whether the patient is HIV positive, and so on). It is almost certainly an overestimate of the true CFR, given that TB incidence has shown a generally declining trend and that there is a lag to death. But it is still very high indeed. Meta study data (see Huddart et al. 2020) estimates a pooled CFR even during the treatment phase of over 5%; these numbers are substantially higher for the significantly prevalent drug-resistant strains.
Compare these rates with the CFRs from Covid-19. The global CFR is orders of magnitude lower for Covid-19 – around 2.1% in all of 2020. Underreporting of cases relative to deaths would bring this number down by another order of magnitude, quite possibly below 1%, but that need not concern us here.
In 2020, the larger number of Covid-19 cases and the smaller CFR (both relative to Covid-19) conspired to create a comparable number of global deaths from the two diseases, as already noted. If the populations of the world were all similar, and churning randomly in their interactions with one another, there would be a far bigger chance of one contracting Covid-19 than TB. However, the sigh of relative relief regarding TB would soon be smothered by the dismaying statistic that one would be far more likely to die of TB conditional on getting it. Indeed, the overall probability of dying of TB in this artificially uniform world is about the same as that from Covid-19. Why, then, are we so obsessed with Covid-19 relative to TB?
Let us get the obvious answer out of the way first, which is that a vaccine for TB – the BCG (bacille Calmette-Guerin) – has been widely administered since the 1920s, so there is nothing to worry about. India, a high-burden country for TB, has an excellent coverage record, with over 90% coverage in 2018. The BCG has an undisputed role in preventing conditions such as tubercular meningitis and other diseases, and it has even been suspected that it might play a serendipitous role in reducing Covid-19 infection. But it is unclear whether, in tropical conditions, the BCG is of any significant efficacy at all as far as pulmonary TB in adults is concerned, and in fact it is fair to say that no adult vaccination against TB is currently available, although research on the subject continues.
Setting that aside, we are effectively in the terrain of diarrhoeal diseases and neonatal infections described earlier. Yes, TB is contagious, of course. TB bacteria are emitted when an individual with active tubercular disease coughs, sneezes, or speaks. Yet, it is far more likely that one will catch TB from a family member or a co-worker than from a stranger. It is especially insulated from spread across socioeconomic categories.
As Figueroa-Munoz and Ramon-Pardo (2008) suggest, “The association between TB and poverty is mediated by overcrowding, poorly ventilated housing, malnutrition, smoking, stress, social deprivation and poor social capital.” In short, TB flourishes in poor, rather than rich, populations. Active tubercular disease is highly segmented. If you are reading this, it is likely that your socioeconomic status goes some way to insulate you against TB. It is therefore also likely (and unfortunate) that you will know of someone who has been infected with, or has even died of, Covid-19. But it is also likely (and equally unfortunate) that you will not know of anyone with active tubercular disease – a disease just as responsible as Covid-19 in its infliction of morbidity and death, and for many more years. Indeed, when was the last time you heard someone advocating social distancing or a lockdown in order to control the spread of TB?
South East Asia, Africa and the Western Pacific account for over 85% of the global case total for TB, and just eight countries – India, Indonesia, China, the Philippines, Pakistan, Nigeria, Bangladesh, and South Africa – account for two-thirds of the same total. A Martian visiting India in 2020 would be excused for disbelieving the evidence of their own eyes – draconian lockdowns designed to isolate and segment the population from exposure to Covid-19 while very little is done by way of drawing public attention or public action to TB in these admittedly difficult times. Indeed, as we observe in the next section, the Covid-19 pandemic may have had serious negative effects on both the tracking and the true incidence of TB cases.
This is yet another instance of what we have called elsewhere “lives versus lives”: specifically, an expression of the battle between visible lives – educated, economically endowed, ever-sensitised to global approval, and above all, scared witless by a deadly disease that respects no economic barriers – and the invisible lives of a silent majority, voiceless and vulnerable, who are already under a chronic and equally deadly burden of disease, quite apart from the enormous economic hardship that is entailed by the assault on Covid-19.
Alas, both across and within countries, a pandemic like Covid-19 assumes a global dimension not so much from considerations of a common fate shared by rich and poor people alike (homilies such as ‘we are all in this together’ come to mind) as from the consideration that the poor are now a source of transmission-threat to the rich. It becomes imperative, then, that a communicable disease like Covid-19 be stopped in its tracks, meriting urgency of attention in a way that other equally or more lethal diseases have not. It should, therefore, come as no surprise that control and mitigation measures such as lockdowns should be an accompanying feature of the global sway exercised by Covid-19. We turn now to this issue.
Lockdown revisited
By lockdown we have in mind a collection of stringent and generalised measures of mitigation and control involving stay-at-home requirements, closure of educational institutions and business enterprises, and embargos on large meetings. In this understanding, lockdown does not include other non-pharmaceutical measures such as testing, tracing, and quarantining (within limits against intrusive surveillance imposed by the right to privacy), mask-wearing, maintaining physical distance, and observing hygienic practices such as hand- and face-washing. The logic underlying lockdown is that it will contribute to ‘flattening the curve’ of infections and deaths, thereby deferring and reducing peak mortality, and thus reducing mortality overall.
A lockdown fundamentally buys time. It flattens the curve, true, but it will also ‘stretch’ the curve, with overall mortality comparisons that are at best ambiguous in the absence of accompanying improvements in health infrastructure. After all, a lockdown-mediated epidemic must generally be a more protracted epidemic.5
A lockdown saves lives if that bought time is well-utilised in setting up appropriate health measures and expanding medical capacity. It is time well-spent if society is determined to provide those complementary responses. A lockdown on its own is invariably costly, including the possibility of lives lost owing to the non-availability or infeasibility of treatment for non-Covid morbidities, the rigours of mass migration of informal-sector workers from urban work-spots to rural homes (as happened in India), starvation and other nutritional conditions caused by the inevitable loss of livelihoods and incomes, suicide caused by the psychological oppression of enforced long-duration stay-at-home measures, and domestic violence.6
In fact, Ray and Subramanian (2020a) signalled these issues at a relatively early stage of the pandemic (28 March), “[T]he general economy-wide costs and the household-specific burdens of a comprehensive lockdown are enormous. A spiralling macroeconomic downturn is an obvious consequence, but what we have in mind is the protracted stress on household incomes, employment, and nutrition, ultimately measured in human lives and not in rupees [emphasis in original].”
And Ray, Subramanian and Vandewalle (2020b) noted the somewhat strange place of politics in this controversy, as manifesting in orthogonally different ways in the first- and third-world countries: “The debate of “lockdown versus economy” assumes very different political hues in economically advanced countries and in India. In the United States, for instance, we support a lockdown without hesitation. The SARS-CoV-2 virus is contagious – far more so than the flu – and even if individual mortality risk could be comparable across COVID and flu (conditional on being infected, that is), the overall strain on the health system is enormous. It is true that the economic effects are also large – certainly so in a high-inequality, restricted-social-net country like the United States – but at least, in that country, one has capacities needed to make people whole: starvation is not first-order. In India, it is first-order. The same progressive support for a lockdown in the “West" may need to be entirely reallocated in a different context.”
There is no contradiction in this seeming schizophrenia across the global North and the global South. It is entirely possible to support a lockdown in the US or in Europe, provided that appropriate measures are taken to compensate individuals for life-threatening social and economic dislocation. Such compensations create a smaller relative burden on the resources of a rich country. Furthermore, given the relatively placid baseline health environment in these countries, the appearance of Covid-19 comes as an enormous negative shock. So, a support for lockdown in the North – one that we share – is entirely reasonable.7
However, these considerations must be reassessed with an unjaundiced eye when we swivel to the South. The very same trade-offs are now twisted and reshaped by different social configurations. Economic dislocation is no longer mere economic dislocation save for a minority of individuals. It is a dire prospect (with lives at stake) for a far greater proportion of the citizenry, perhaps for a majority of them. The corresponding compensation must be far more comprehensive, certainly relative to the available resources of a poor country.
Elsewhere, we have developed these observations in detail (see Ray and Subramanian 2020b) and see little point in adding to those considerations here. It suffices to say that a case can still be made for a lockdown, although the stakes are far higher. Rather, what we wish to remark upon here is that there is no such thing as the socially optimal policy. As we have observed (Ray and Subramanian 2020b), “whose welfare is often a far more important question than the textbook criterion of ‘market failure’ relative to some universally accepted social welfare function”. Or, to invoke our Animal Farm perspective, all communicable diseases may indeed be equal, but some are more equal than others. It depends on whose lives are directly threatened, and by which disease, and the voice that is possessed by each group to ward off that threat.
Returning to TB, a disease that is indisputably agreed to be a scourge of the poor, it is bad enough that the public awareness of contagion created by Covid-19 extends not at all to TB or other diseases, that the only vaccine developed for TB and in use since 1921 is of very limited efficacy, and that new research on the subject proceeds at a glacial pace relative to the ‘warp speed’ reactions we have (thankfully) seen for Covid-19.
But what is worse is that the effort devoted to Covid-19 appears to have significantly affected the tracking and notification of TB cases.
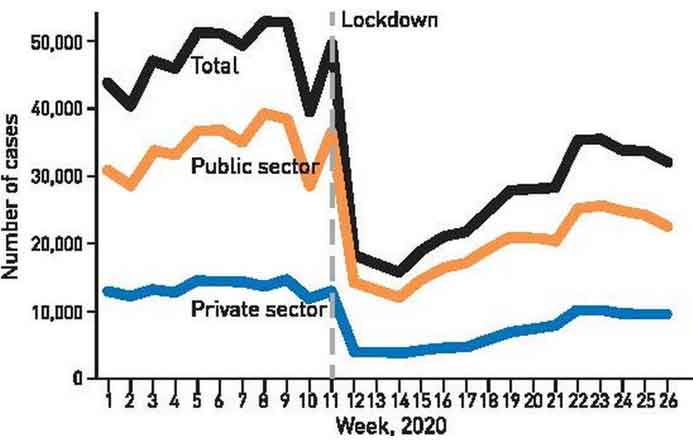
The Government of India requires that all cases of TB be notified, whether or not they are detected in a private or public health facility. Average notifications in the calendar year 2019 were slightly in excess of 200,000 cases a month: this trend continued into January and February of 2020 at exactly the same level – an average of 205,500. In March and April following the imposition of the national lockdown, the average fell to 125,500 a month, a drop of close to 40%. This is a huge fall in notifications, and it means that in just two months 150,000 cases of TB went ‘missing’. Figure 1 is reproduced from the 2020 Global Tuberculosis Report and shows how these notifications fell on a weekly basis in the period following the lockdown.
Figure 1. Weekly tuberculosis notifications before and after the lockdown in India
It should be noted that this dramatic fall in notifications was by no means restricted to India and occurred globally (see, for example, Figure 3.3 in the Global Tuberculosis Report 2020). In fact, it is not our intention to blame the Government of India at every step of the way. India has been a leading player in the global fight against TB. Rather, it is a systemic problem. When a disease that afflicts the rich muscles its way onto the international stage, the pressures set up are immense, and the resulting political-economy drama that plays out can inexorably take its toll on diseases that largely affect the poor.
Having said that, a poorer country government would merit praise if it were to stand up to these pressures instead of painlessly succumbing to them.
The effect of Covid-19 on the war against TB may well be very large. The Global Tuberculosis Report (2020) observes: “If the number of people with TB detected and treated were to fall by 25-50% over a period of three months – a range considered plausible based on data from several high TB burden countries – there could be between 200,000 and 400,000 excess TB deaths in 2020, bringing the total to about 1.6-1.8 million…. A three-month lockdown combined with a protracted (10-month) restoration of services could cause an additional 1.4 million TB deaths between 2020 and 2025.”
These are very large estimates and rely entirely on unreported cases as well as the projected disruption of essential services to combat TB. Such services include manpower, the reallocation of machines used in testing (GeneXpert machines that are used to diagnose TB can be and have been deployed for Covid-19 testing in several countries), and reduced access to health clinics and medication.
We can only begin to estimate how the severe worsening of economic conditions and accompanying increase in undernutrition might affect the future incidence of TB. The Stop TB Partnership study (2020) has indicated that the Covid-19 pandemic could result in an additional 6.3 million TB cases worldwide between 2020 and 2025.
Disease versus disease
We have deliberately set off disease against disease. We know, as do many others, that the Covid-19 lockdown has had other consequences that bear on human life not just via worsened disease outcomes. Our focus has been to show that even from the narrow perspective of disease versus disease, Covid-19 has extracted a toll.
It is not difficult to see that an unqualified international approbation for a lockdown to battle with Covid-19 could have fed, in poorer countries, into what has been called a “perverse politics of visibility” – harsh and unyielding on high-profile measures such as lockdowns and uncaring on the collateral damage that has been wreaked on the poor.
In the interests of fairness, international opinion on lockdowns in poorer countries has not always been unqualified. The importance of alleviating the harsher aspects of lockdown, and of being mindful of these, have not gone unaddressed.8
But such caveats and reservations have often been offered after the fact and they fail to remove the sense that they constitute something of an effort to hedge one’s bets. In many ways, the view seems to be that lockdown was necessary, even if not sufficient. Having said that, ‘necessary but not sufficient’ is not the same thing as a plea to ‘avoid a lockdown if the capacity or willingness to alleviate collateral damage is absent’.
Overall, therefore, it is fair to assert that the geopolitics of Covid-19 has been one in which it is the interests of the North that have been prioritised, and within countries, those of the relatively affluent constituency of citizens who make opinion and influence policy.
Conclusion
Is it this post’s contention, then, that the Covid-19 pandemic is largely a matter of much ado about nothing? Very far from it – not least when we consider the possibility that Covid-19 mortality, especially in the poorer countries of the world, has probably been considerably underestimated (an issue we do not get into in the present analysis).
No, we believe that the pandemic is a deadly serious affair. And it is precisely because of the gravity involved, that it is right and necessary to assert that despite the apparent sentiment that ‘we are all in this together’, the global burdens of Covid-19 and the global benefits of anti-Covid-19 policy have been skewed against the poorer nations of the world – and within nations, against the poor and the vulnerable. The demand is not for any sort of ‘compensatory discrimination’ in favour of the poor: the claim, rather, is that not even the requirements of a neutral, disinterested fairness have been observed in the global response to the Covid-19 epidemic.
The intention is not to mount an unrealistic objection to self-interest but to suggest that there is a case for some sort of even-handed balance between self- and other-interest. In the end, one is perhaps best enlightened, in the present context, not by Shakespeare but by the Bible: “Ye shall do no unrighteousness in judgment. Thou shalt not respect the person of the poor, nor honour the person of the mighty, but in righteousness shalt thou judge thy neighbour”.9
The authors wish to state that this post has benefitted from comments by Thomas Pogge on an earlier version, though he is not implicated in any of the views expressed here.
This is an edited version of an essay that was originally published in Frontline. Permission to reproduce the article is gratefully acknowledged.
I4I is now on Telegram. Please click here (@Ideas4India) to subscribe to our channel for quick updates on our content.
Notes:
- Other resources on Covid-19 include the British Medical Journal, Cambridge University Press, the Centers for Disease Control and Prevention, the Chinese Medical Association, Cochrane, Elsevier, the European Centre for Disease Prevention and Control, the Journal of the American Medical Association, The Lancet, LitCOVID: U.S. National Library of Medicine, the New England Journal of Medicine, Oxford University Press, PLOS COVID-19 Research, The Public Library of Science, Public Health England, Science, Springer Nature, Social Science Research Network SSRN (preprints), and Wiley: this list could probably be doubled with ease.
- These are somewhat rough estimates: WHO data on the 4C diseases we accessed are presented on line-charts, without precise accompanying numbers; we measured these with a foot-rule against a normalised scale.
- The importance of providing per capita numbers for Covid-19 has been noted by Kaushik Basu (2020).
- China is classified as an upper middle-income country and therefore belongs to the set of richer countries.
- See Raju (2020) for a detailed exposition of this important point.
- We do not deal here with the question of a reasonable alternative to stringent and comprehensive lockdowns – the question has been dealt with elsewhere (for example, in Ray et al. 2020).
- We should note that even in the North, there has been controversy regarding the extent of lockdown and related measures. The so-called Great Barrington Declaration, drafted by Martin Kulldorf, Sunetra Gupta, and Joy Bhattacharya on 3 October 2020, notes that “current lockdown policies are producing devastating effects on short and long-term public health. The results (to name a few) include lower childhood vaccination rates, worsening cardiovascular disease outcomes, fewer cancer screenings, and deteriorating mental health – leading to greater excess mortality in years to come, with the working class and younger members of society carrying the heaviest burden…Keeping these measures in place until a vaccine is available will cause irreparable damage, with the underprivileged disproportionately harmed”. In contrast, an opposing statement called the John Snow Memorandum (see Alwan et al. 2020), released on 14 October, reads in part: “the evidence is very clear: controlling community spread of Covid-19 is the best way to protect our societies and economies until safe and effective vaccines and therapeutics arrive within the coming months.” Both declarations have received considerable support and endorsement but are not our main focus in this post.
- For instance, Ramanan Laxminarayanan the Director of The Center for Disease Dynamics, Economics and Policy, Washington, DC, writes: “The [Indian] government’s decision to impose the lockdown was necessary to mitigate the inevitable spread of the disease…A lockdown was the only option to control the disease…The lockdown has most likely saved millions of lives, but the bold public health actions of the government should be matched by similar efforts to ensure that the pandemic does not generate a secondary hunger and poverty crisis” (Laxminarayanan 2020).
- Leviticus 19:15, King James Version.
Further Reading
- Alwan, Nisreen A et al. (2020), “Scientific Consensus on the COVID-19 Pandemic: We Need to Act Now”, The Lancet, 396(10260).
- Basu, K (2020), ‘Who’s Afraid of COVID-19?’, Project Syndicate, 6 May.
- Cinelli, Matteo, Walter Quattrociocchi, Alessandro Galeazzi, Carlo Michele Valensise, Emanuele Brugnoli, Ana Lucia Schmidt, Paola Zola, Fabiana Zollo and Antonio Scala (2020), “The COVID-19 Social Media Infodemic”, Scientific Reports, 10(16598).
- Dixit, A (2020), ‘R0 for Covid-19 research: An Early Estimate and Policy Implications’, Unpublished Manuscript, Princeton University.
- Figueroa-Munoz, Jose I and Pilar Ramon-Pardo (2008), “Tuberculosis Control in Vulnerable Groups”, Bulletin of the World Health Organization, 86(9): 733-735.
- Huddart, Sophie, Anita Svadzian, Vaidehi Nafade, Srinath Satyanarayana and
- Madhukar Pai (2020), “Tuberculosis case fatality in India: a systematic review and meta-analysis”, BMJ Global Health, 5:e002080.
- Kulldorf, M, S Gupta and J Bhattacharya (2020), ‘Great Barrington Declaration’.
- Laxminarayanan, R (2020), ‘What India Needs to Fight the Virus’, The New York Times, 27 March.
- Mannava, Priya, John CS Murray, Rokho Kim and Howard L Sobel (2019), “Status of water, sanitation and hygiene services for childbirth and newborn care in seven countries in East Asia and the Pacific”, Journal of Global Health, 9(2): 1-10.
- Raju, S (2020), ‘Did the Indian Lockdown Avert Deaths?’, Social Science Research Network.
- Ray, D and S Subramanian (2020a), ‘Is There a Reasonable Alternative to a Comprehensive Lockdown?’, Ideas for India, 28 March 2020.
- Ray, D and S Subramanian (2020b), ‘India’s Response to Covid-19 is a Humanitarian Disaster’, The Boston Review, 16 July 2020.
- Ray, Debraj and S Subramanian (2020c), “India’s Lockdown: An Interim Report”, Indian Economic Review, 55(S1): 31–79.
- Ray, D, S Subramanian and L Vandewalle (2020), ‘India’s Lockdown’, Center for Economic Policy Research Policy Insight No. 102.
- Stop TB Partnership (2020), ‘The potential impact of the COVID-19 response on tuberculosis in high-burden countries: a modelling analysis’, Stop TB Partnership in collaboration with Imperial College, Avenir Health, Johns Hopkins University and USAID.
- United Nations General Assembly (2020), ‘Report of the Special Rapporteur on the right to privacy’, New York, United States.




 23 February, 2021
23 February, 2021 





Comments will be held for moderation. Your contact information will not be made public.