While a large, multidisciplinary literature focusses on disparities in physical health across social groups, the mental health dimension remains invisible. Analysing data from a WHO survey conducted in six Indian states in 2007-2008, this article shows that Scheduled Castes and Muslims have worse (self-reported) mental health than upper-caste Hindus – even after accounting for differences in education and asset ownership.
In May 2019, Payal Tadvi, a medical student from a tribal Muslim community, died by suicide, after facing persistent caste-related discrimination. This is not an isolated incident. The violence against people protesting the Citizenship Amendment Act left more than 50 dead, of whom two thirds were Muslim. In light of the persistent caste- and religion-based discrimination, it is important to understand how caste and religion shape mental health outcomes.
Background
A large, multi-disciplinary literature has been concerned with understanding disparities in health by ethnicity, gender, socioeconomic status, and caste. This includes infant mortality (Guillot and Allendorf 2010, Spears and Geruso 2018, Ramaiah 2015), child height (Coffey et al. 2019), and the use of health services (Baru et al. 2010). In this context, the association between belonging to marginalised groups and lower mental health at a community level is especially important. According to the Indian National Mental Health Survey (2015-16), 10% of the Indian population suffer from common mental disorders (Gururaj et al. 2016). Because reporting poor mental health is stigmatised, the actual number is likely to be higher. In an interview with Surinder Jodhka (Professor of Sociology, Jawaharlal Nehru University), psychiatrist Sushrut Jadhav of University College London, argues that mental health dimensions of caste “remain invisible to both academia and popular culture” (Jodhka and Jadhav 2012). In recent work, we seek to address this gap in evidence by analysing disparities in mental health by social groups in India (Gupta and Coffey 2020). To our knowledge, this is the first such study that uses population-representative data.
Data
We use data from the World Health Organization’s (WHO) Study of Global Ageing and Adult Health (SAGE) conducted in six large Indian states in 2007-2008. The WHO-SAGE is representative of the adult population in these states, and collected information on mental health outcomes, social group, and socioeconomic status. The two outcomes that we analyse from these data are:
- Overall in the last 30 days, how much of a problem did you have with feeling sad, low, or depressed? None, mild, moderate, severe, or extreme?
- Overall in the last 30 days, how much of a problem did you have with worry or anxiety? None, mild, moderate, severe, or extreme?
Approach
Our study focusses on the following questions:
- Are there are disparities in self-reported mental health indicators between Scheduled Castes (SCs) and upper-caste Hindus, and between Muslims and upper-caste Hindus?
- What is the magnitude of these disparities?
- To what extent can they be explained by disparities in socio-economic status?
In order to answer these questions, we use two empirical strategies – 1) a 'non-parametric reweighting standardisation' technique that tells us what mental health outcomes among Muslims and SCs would be if they had the same distributions of education and asset wealth as as upper-caste Hindus, and 2) a 'regression analysis' that shows that after controlling for socioeconomic status differences, SCs and Muslims have worse mental health outcomes.
Mental health outcomes for marginalised groups
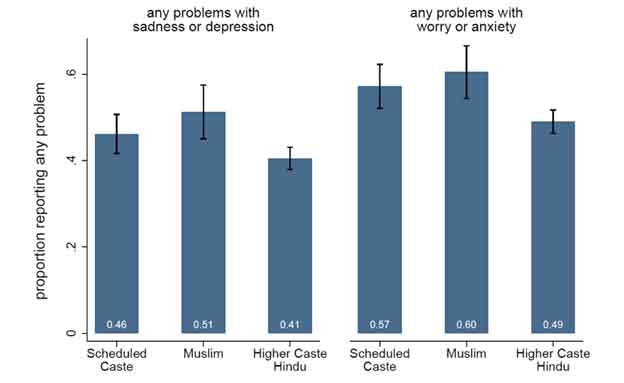
For both outcomes, SC and Muslim respondents had worse mental health than upper-caste Hindu respondents (Figure 1). About 41% of upper-caste Hindu respondents, 46% of SC respondents, and 51% of Muslim respondents reported being mildly, moderately, severely, or extremely depressed in the last month. Slightly less than half of upper-caste Hindu respondents, 57% of SC respondents, and 60% of Muslim respondents reported facing anxiety in the last month.
Figure 1. Self-reported mental health outcomes, by social group
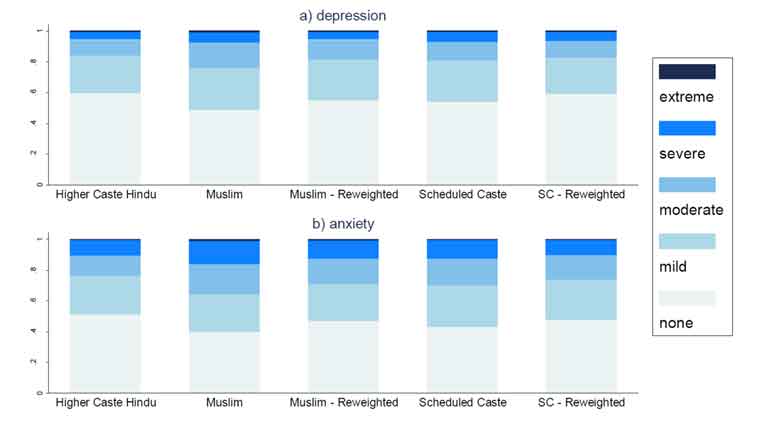
Figure 2 plots distributions of self-reported mental health based on the reweighting technique described above. The reweighted distributions represent counterfactual distributions of mental health outcomes that answer the question: what would the mental health outcomes of Muslims (or SCs) look like if they had the same distribution of assets and educational attainment as upper-caste Hindus?
Figure 2. Distribution of self-reported mental health outcomes
The reweighted distributions of SCs and Muslims in Figure 2 are closer to the distribution of mental health outcomes – in the range of none to extreme – among upper-caste Hindus than the unweighted distributions. However, for most outcomes, there is still a visible mental health gap. The exception is the gap for depression between SCs and upper-caste Hindus, which appears to be entirely explained by differences in assets and educational attainment.
Throughout the empirical analysis, we find that Muslims are substantially more likely to report sadness and anxiety, as compared to upper-caste Hindus, even after controlling for age, education, assets, expenditure, state of residence, and rural residence.
Concluding remarks
SCs and Muslims have worse self-reported mental health than upper-caste Hindus. In most cases, these gaps remain even after accounting for the fact that SCs and Muslims have less education and own fewer assets.
Considering this analysis uses data from 2007-2008, gaps between upper-caste Hindus and minorities may be even larger today considering the recent rise in violence against minorities in India, and their further marginalisation. We think that the increase in prejudice against Muslims (Council on Foreign Relations 2020), the rise in incidents of lynching, the National Register of Citizens exercise in Assam, protests related to the Citizenship Amendment Act, subsequent riots in Delhi, and related events have likely increased levels of depression and anxiety among Muslims, and thereby increased the gap in mental health outcomes between Muslims and upper-caste Hindus. In order to better understand mental health disparities in 2020, we would need more recent data from more states. Finally, further work to understand the links among discrimination, violence, and mental health outcomes is crucial.
What are the implications of this work documenting mental health disparities in India? Existing policy frameworks to challenge social inequalities in India prioritise affirmative action and redistributive policies. There is an urgent need to supplement these frameworks with policies that take stronger stances against violence and discrimination. Mental health policies can also prioritise a preventive approach. To the extent that discrimination and violence contribute to depression and anxiety in India, reducing them would improve overall mental health. This is especially relevant in low-resource settings such as India, where access to mental healthcare is extremely limited.
This is the last of a three-part series on mobile phone survey methods, measuring mental health and disparities in mental health in India.
Further Reading
- Baru, Rama, Arnab Acharya, Sanghmitra Acharya, AK Shiva Kumar and K Nagaraj (2010), “Inequities in access to health services in India: Caste, class and region”, Economic and Political Weekly, 45(38): 49–58.
- Coffey, Diane, Ashwini Deshpande, Jeffrey Hammer and Dean Spears (2019), “Local social inequality, economic inequality, and disparities in child height in India”, Demography, 56: 1427–1452.
- Guillot, Michel and Keera Allendorf (2010), “Hindu-Muslim differentials in child mortality in India”, Genus, 66(2): 43-68.
- Gupta, Aashish and Diane Coffey (2020), “Caste, Religion, and Mental Health in India”, Population Research and Policy Review.
- Gururaj, G, M Varghese, V Benegal, GN Rao, K Pathak, LK Singh and R Misra (2016), National mental health survey of India, 2015-16.
- Jadhav, Sushrut and Surinder Jodhka (2012), “Caste, culture, and clinic” Seminar, 633.
- Lindsay Maizland (2020), ‘India’s Muslims: An Increasingly Marginalized Population’, Council on Foreign Relations, 20 August.
- Ramaiah, Avatthi (2015), “Health status of Dalits in India”, Economic and Political Weekly, 50(43): 70–74.
- Spears, Dean and Michael Geruso (2018), “Neighborhood sanitation and infant mortality”, American Economic Journal, 10(2): 125–162.




 13 November, 2020
13 November, 2020 





Comments will be held for moderation. Your contact information will not be made public.