While India’s maternal mortality rate declined substantially during 2004-2006 to 2014-2016, at an annual rate of 5%, the reduction is still short of what is required to achieve the National Health Policy target. Jithin Jose proposes a four-pronged strategy to sustain and accelerate the decline, RAFT – review of medical records, death certificates or autopsy reports of mothers; access to quality and respectful healthcare for women; funding for infrastructure, medicines, and interventions in the labour room; and training of personnel.
As per the Sample Registration System (SRS) data, India has achieved the Millennium Development Goal (MDG) 5A, which stated that all countries should reduce Maternal Mortality Rate MMR by 75% of their respective 1990 figures by 20151. However, other sources seem to put the MMR at a higher figure2. Regardless, we have seen a pan-India decline in (MMR), at an annual rate of 5% during 2004-2006 to 2014-2016. In March 2017, with the aim of achieving the Sustainable Development Goals (SDGs)3, Government of India proposed the National Health Policy (NHP), which set an MMR target of 100 to be achieved by 2020. This means that India would have to reduce its MMR at an annual rate of 5.75% in the coming years, which is more than its annual average reduction during 2004-2006 to 2014-2016.
However, achieving this target would be an uphill task, as any further reductions in the MMR at the national level would require ending preventable maternal mortality. Moreover, considerable amount of resources need to be instituted for per unit of count reduction in order to sustain and accelerate India’s successes. This would require continuous reductions in both mortality and morbidity, with complementary improvements along the continuum of care for women (World Health Organization (WHO), 2015). Within this context, strengthening of health systems and continuous learning; enabling and mobilising individuals and communities; and advancing quality, respectful care have been identified as critical to making progress towards this goal (United States Agency for International Development (USAID), 2014).
The RAFT strategy
In this post, I propose a four-pronged strategy, RAFT, that is, Review of medical records, death certificates or autopsy reports of mothers; Access to quality and respectful healthcare for women, Funding for infrastructure, medicines, interventions in the labour room; and Training for personnel.4 This strategy encompasses the three goals mentioned above and is to be implemented at the state level with strong backing from the Centre.
Review of medical records, death certificates, and autopsy reports will ensure that the underlying causes of maternal deaths are understood. In such a review, each and every maternal death case sheet in a particular year is examined by an expert committee comprising obstetric and non-obstetric assessors. The responsibility of sending the details of every maternal death lies with the hospital. The personal details of the patient and the presiding physician are kept confidential so as to prevent any bias in understanding the actual factors that caused the death of the mother. This process is currently being followed regularly in Kerala since the initiation of Confidential Review of Maternal Deaths (CRMD) in 2004, with support from WHO (Paily 2014). During that period, for Kerala, where 99.3% of deliveries were institutional5, such a process was feasible as the probability of all maternal deaths being reported and captured was high. However, this might not be the case with other Indian states currently, especially the ones that are part of the Empowered Action Group (EAG)6 where the average rate of institutional birth is around 72.6% (NFHS-4). Therefore, in such cases, an alternative would be a review of the death certificate report or the autopsy report. Since the causes of maternal deaths may differ across regions due to various factors, each states should make this process mandatory. For EAG, such a process is necessary, given the dismal performance in terms of reducing MMR (See Figure 1 below).
Figure 1. MMR by state groups
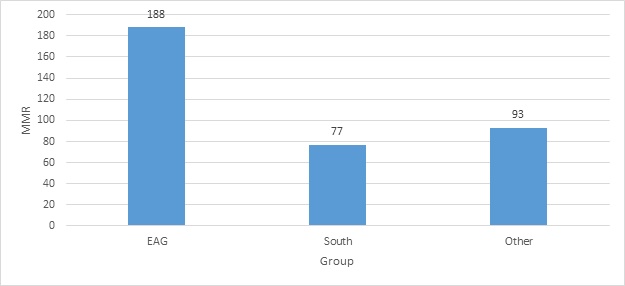 Source: SRS 2014-16 estimates.
Source: SRS 2014-16 estimates. Note: EAG refers to states that are a part of the Empowered Action Group
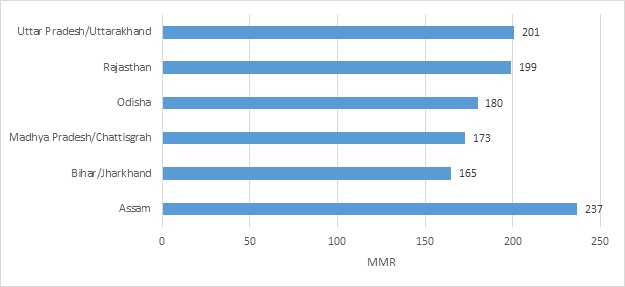
Figure 2: MMR in EAG states
Secondly, access to healthcare in terms of maternal health should be given to all women. This encompasses a broad spectrum of interventions ranging from educating and empowering women with regard to maternal health; family planning initiatives; addressing inequities in access to and quality of sexual, reproductive, and maternal healthcare; and enhanced mobilisation of individual and communities. A good starting point would be to learn from past experiences through a thorough review of existing demand-side interventions7. This will aid in identifying major gaps in the provision and access of basic maternal healthcare that impede reduction in maternal mortality, and guide stakeholders in adopting practices that have been proven to work. For example, assessments of the Janani Suraksha Yojana (JSY)8 show that it had an impressive effect on rates of institutional delivery, but no effect on maternal mortality (Lim et al.2010, Randive et al. 2013, Paul et al. 2010). Certain studies show that targeted delivery of messages through media campaigns was found to be more effective than peer education, and women receiving health education were less likely to experience pregnancy and labour-related issues (Banerjee et al. 2013, Leon et al. 2014, Achyut et al. 2016). Moreover, such interventions can be effectively complemented by community-led interventions to hold the government and providers accountable, in case the quality of existing services falls. For example, Subha et al. (2012) show how following local protests against a high number of maternal deaths in 2010 in Barwani district in Madhya Pradesh, a maternal death review was conducted by civil society to investigate the 27 maternal deaths reported in the district.
Furthermore, in order to save mothers’ lives, we need to provide them with skilled obstetric care, which can be accessed in facilities. But what happens once you have ensured that mothers opt for institutional deliveries and these facilities turn out to be ill-equipped? Muldoon et al. (2011) finds that almost one-third of rural health sub-centres lack regular water and electrical supply, elevating the risk of infection ( Neil et al. 2017). Additionally, Hulton et al. (2007), Ghodki and Sardesai (2014), Jadon and Bagai (2014) show that one-third of PHCs lacked labour rooms, and some hospitals lacked essential drugs, performed surgical procedures such as Caesarean sections with no onsite blood banks or reliable anesthetics and sometimes without health professional, further increasing the risk of unmanaged pregnancy complications (Neil et al. 2017). In such cases, the review process would not be effective unless funding is set aside by each state for improving infrastructure and training staff to tackle major causes of maternal deaths across all delivery points9.
Finally, none of the above processes would work efficiently without continuously updating personnel knowledge related to the management of labour and delivery and also in terms of improving the quality of “respectful care”. Das et al. (2015, 2012) find that less than one-third of providers in India adhere to clinical guidelines and fewer than half of clinical interactions result in correct diagnoses and treatment (Neil et al. 2017). Hence, a direct complement to review, access, and funding is a homogenised emergency obstetric care (EMOC) training programme, which should be initiated at the state level. It should be directed at two levels of caregivers, that is, at the facility level for obstetricians, nurses and nursing attendants/cleaners10, and at the frontline worker level for accredited social health activists (ASHA) and auxiliary nurse midwives (ANM). Ideally this training programme should cover evidence-based clinical guidelines and techniques to ensure that caregivers are updated with the latest information and best practices. Anecdotal evidence has shown that training and feedback reduces unnecessary and potentially harmful practices, improves access to skilled maternal and neonatal care in rural areas, and helps in managing maternal complications with and without the need for referral (Iyengar and Iyengar 2009, Jejeebhoy et al. 2011, Iyengar et al. 2014). Training clinicians and programme managers also improve in adherence to evidence-based practices (Iyengar et al. 2014).
Kerala’s experience
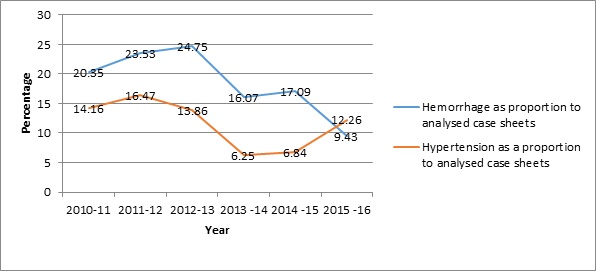
In Kerala, the CRMD committee consistently reviewed an average of 50% case sheets related to maternal deaths during 2004-2009 (Smith 2014). Upon review, the major causes were identified to be Post-Partum Hemorrhage (PPH) and Pregnancy Induced Hypertension (PIH). As a result of this process, Kerala initiated the quality standards programme. This programme consisted of a training based on a set of 10 evidence-based guidelines to reduce PPH- and PIH-related deaths. In April 2013, six public delivery points11 were provided with funds to purchase adequate medicines and equipment along with training on quality standards to tackle hemorrhage and hypertension as part of the Emergency Obstetric Care and Life Support (EMOCALS)12 training programme. This brought down the occurrence of PPH and PIH deaths and also reduced referrals in the hospitals where these training programmes were piloted.
As per the latest CRMD data provided to me by the Kerala Federation of Ostetricians and Gynecologist (KFOG), the proportion of deaths related to PPH amongst the cases reviewed fell from 20.4% in 2010-11 to 9.4% in 2015-16. PIH as a cause of maternal death also declined during this period. As we can see in Figure 3 below, it declined from 14.1% in 2010-11 to 12.3% in 2015-16. However, it had declined considerably till 2014-15. The huge jump for the year 2015-16 can be attributed to many factors like shortage of medicines and lack of trained staff, all which points towards administrative apathy. In both cases, we can observe a fall in the proportion of maternal deaths for PPH and PIH around 2013-14. Additionally, during this period, the average proportion of maternal death cases reviewed by the committee out of the total maternal deaths cases was 66.8%. This is an increase from the previous average of around 50% during 2004-2009.
Figure 3: Hemorrhage and hypertension deaths
Conclusion
Kerala’s example should pave the way for more states to adopt RAFT as a viable strategy to improve MMR. This experience also points out where the strategy could fail especially if the administration becomes lax in its implementation. Moreover, only about one-third of the case sheets being reviewed between 2010-2016 in Kerala, is indicative of incomplete reporting in the case sheets by the physicians responsible. This will be a potential logistical problem that the states might face while implementing the Review component of the strategy in the beginning. Therefore, in this context, the central government should support the states, firstly in their efforts to adopt this strategy, especially the CRMD process by institutionalising it and making it mandatory for all public hospitals to report maternal deaths with complete documentation to a CRMD committee at the state level13. This can be further extended to private hospitals over a period of time. In addition, special attention should also be given to improving documentation practices among physicians and their interns (house surgeons)14. Within this capacity, a central mandate conveying such responsibilities to relevant obstetrician and gynecologist unions15 in each state would be a way to go. In this process, the states could work with these unions to set up a CRMD committee. Such unions could decide on the methodology for the review committees to follow, given the situation in a particular state, that is, review of case sheet, death report or autopsy reports. Secondly, the Centre should also extend funds to each state for the purchase of necessary equipment, improving infrastructure, and for training labour-related personnel. Presently, LaQshya and Dakshata programmes under the aegis of the National Health Mission are steps in that direction. Thirdly, an expert panel should be set up at the national level to review the present course structure of the EMoC (Emergency Obstetric Care) initiative16 which all the states could follow, thereby ensuring homogeneity in training content across the country. Fourthly, a separate cadre of obstetric nurses should also be formed. This would ensure that such trainings do not suffer from administrative bottlenecks like staff rotation. This would help in retaining staff trained in such methods within the delivery unit.
Therefore, if the administration is able to adopt the core principles of RAFT and provide necessary support to states for its implementation, we can expect India to achieve its MMR target set by the SDGs.
This post is based on the author’s observations from the ongoing 3ie-funded IFMR-LEAD study titled “Impact Evaluation of an Intervention to Reduce Maternal Mortality in Kerala, India”, being conducted in partnership with the National Health Mission, Kerala.
Notes:
- As per the SRS, MMR for 2014-2016 is 130. As per the Ggovernment of India the target was 140
- The Central Intelligence Agency (CIA) Factbook, World Bank, UNICEF (United Nations Children’s Emergency Fund), WHO (World Health Organization) have all calculated the MMR as 176 (2015 estimate).
- So far, Kerala, Maharashtra, and Tamil Nadu have achieved the goal set by the SDGs
- The components within this strategy are complements and the overall objective may not be realised if these are implemented individually or as substitutes for one another.
- This figure is from 2005-2006, when National Family Health Survey-3 (NFHS-3) was published. Presently, it is 99.9% as per NFHS-4.
- In India, the nine socioeconomically backward states of Assam, Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Orissa, Rajasthan, Uttaranchal, and Uttar Pradesh, referred to as the Empowered Action Group (EAG) states (Arokiasamy 2008).
- Demand-side interventions focus on reducing barriers to seeking maternal healthcare and empowering community members to seek higher quality care. These interventions include efforts to inform women, families, and communities about their rights to high-quality care.
- In order to reduce neonatal and maternal deaths, JSY scheme provides a cash incentive for women to deliver at healthcare facilities. It covers about 9·5 million women per year, making it the largest conditional cash transfer programme in the world.
- For example, if the major causes have been identified as PPH, PIH, and Sepsis, drugs like uterotonics and anti-hypertensive; instruments like oxygen masks, delivery kits with blood-absorbing pads, sepsis kits, and anti-shock garments; and basic infrastructure like blood storage unit or blood bank, water, electrical supply, and so on, are the most basic supplies that any delivery point should have without which it would be difficult for the personnel to dispense quality treatment
- Training of obstetricians, nurses, and nursing assistants together, does not seem to lead to any improvements in the quality of work of the nursing assistants; the responsibilities of doctors and nurses are starkly different from that of the nursing assistants. A separate module for nursing assistants should be created, which directly deals with their work and training should be imparted to them on the basis of this module.
- General Hospital Ernakulam, DH Peroorkada, Taluk Hospital Chirayinkeezhu, CHC Kanyakulangara, Women & Children Hospital, Thycaud and SAT Hospital
- Also referred to as the “Quality Standards Programme”.
- In this process, a centralised Pregnancy Mortality Surveillance System (PMSS) could be set up, on the lines of the existing Hospital Management Information System (HMIS) under the NHM, which could ideally be a database of information on maternal deaths.
- It has been observed that house surgeons are sometimes given the responsibility of filling up information in the case sheets of mothers. This practice is part of their training and helps them to understand the documentation processes so that they are fully aware of their roles and responsibilities as future Obstetricians/Gynecologists (OBGYN).
- The Federation of Obstetric and Gynaecological Societies of India (FOGSI) is the professional organisation representing practitioners of obstetrics and gynaecology in India. It comprises 241 member societies and over 33,000 individual members spread across the country.
- The EMOC is a joint initiative of the Ministry of Health and Family Welfare, FOGSI, and the Indian College of Obstetricians and Gynecologists.
Further Reading
- Achyut, Pranita, Aimee Benson, Lisa M Calhoun, Meghan Corroon, David K. Guilkey, Esset Kebede, Peter M Lance, Anurag Mishra, Priya Nanda, Rick O’Hara, Ranajit Sengupta, Ilene S Speizer, John Stewart and Jennifer Winston (2016), “Impact Evaluation of the Urban Health Initiative in Urban Uttar Pradesh, India”, Contraception, Vol. 93, No. 6, pp. 519–525, 31 February.
- Arokiasamy, Perianayagam and Abhishek Gautam (2008), “Neonatal mortality in the empowered action group states of India: Trends and Determinants”, Journal of Biosocial Science [Abstract], 40(2): 183-201.
- Banerjee, Sushanta K, Kathryn L Andersen, Janardhan Warvadekar, and Erin Pearson (2013), “Effectiveness of a Behavior Change Communication Intervention to Improve Knowledge and Perceptions about Abortion in Bihar and Jharkhand, India”, International Perspectives on Sexual and Reproductive Health, Vol. 39, No. 3, pp. 142–151, 15 October.
- Iyengar, Kirti, Motilal Jain, Sunil Thomas, Kalpana Dashora, William Liu, Paramsukh Saini, Rajesh Dattatreya, Indrani Parkerand, and Sharad Iyengar (2014), “Adherence to Evidence Based Care Practices for Childbirth Before and After a Quality Improvement Intervention in Health Facilities in Rajasthan, India”, BMC Pregnancy and Childbirth, Vol. 14, No. 270, August. Available here.
- Iyengar, Kirti and SD Iyengar (2009), “Emergency Obstetric Care and Referral: Experience of Two Midwife-Led Health Centres in Rural Rajasthan, India”, Reproductive Health Matters, Vol. 17, No. 33, pp. 9–20, June. Available here.
- Jejeebhoy, SJ, S Kalyanwala, AJF Zavier, R Kumar, S Mudle, J Tank, R Acharya, and N Jha (2011), “Can Nurses Perform Manual Vacuum Aspiration (MVA) as Safely and Effectively as Physicians? Evidence from India”, Contraception, Vol. 84, No. 6, pp. 615-621, December. Available here.
- Khanna, Renu, Subha Sri B, and Sarojini N (2012), “An investigation of maternal deaths following public protests in a tribal district of Madhya Pradesh, central India”, Reproductive Health Matters, 20(39): 11-20, DOI: 10.1016/S0968-8080(12)39599-2, June.
- Leon, Federico R, Rebecka Lundgren, Irit Sinai, Ragini Sinha and Victoria Jennings (2014), “Increasing Literate and Illiterate Women’s Met Need for Contraception via Empowerment: A Quasi-Experiment in Rural India,” Reproductive Health, Vol. 11, No. 74,21 October.
- Lim, SS, Lalit Dandona, Joseph A Hoisington, Spencer L James, Margaret C Hogan, and Emmanuela Gakidou (2010), “India’s Janani Suraksha Yojana, a Conditional Cash Transfer Program to Increase Births in Health Facilities: An Impact Evaluation”, Lancet, Vol. 375, pp. 2009–2023, 5 June.
- Paily, VP, K Ambujam, V Rajasekharan Nair, and B Thomas (2014), “Confidential Review of Maternal Deaths in Kerala: a country case study”, BJOG, 121: (Suppl. 4): 61-66 [Abstract].
- Paul, Vinod K (2010), “Conditional cash transfers for in-facility deliveries”, The Lancet,375(9730):1943–1944, doi: 10.1016/S0140-6736(10)60901-4, 5 June.
- Randive, B, V Diwan, and A De Costa, ‘India's Conditional Cash Transfer Program (the JSY) to Promote Institutional Birth: Is There an Association Between Institutional Birth Proposition and Maternal Mortality?’, PLOS ONE, Vol. 8, No. 6, June 2013.
- Smith, H et al. (2014), ‘Confidential Review of Maternal Deaths (CRMD) in Kerala, India’, World Health Organization.
- So O'Neil, Katie Naeve, and Rajani Ved (2017), ‘An Examination of the Maternal Health Quality of Care Landscape in India’, Mathematica Policy Research, 2 March.
- USAID (2014), ‘Ending preventable maternal mortality: USAID Maternal Health Vision for Action’, June.
- WHO (2015), ‘Strategies towards ending preventable maternal mortality’, February.




 11 June, 2018
11 June, 2018 




By: Sobia jan 16 February, 2021
In India, the nine socioeconomically backward states of Assam, Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Orissa, Rajasthan, Uttaranchal, and Uttar Pradesh, referred to as the Empowered Action Group (EAG) states, lag behind in the demographic transition and have the highest maternal mortality rates in the country (Arokiasamy 2008). This reference is wrong this is research for neonatal deaths, u have write it as maternal death.