Although the prevalence of depression may have adverse economic impacts, especially in developing countries, treatment options in India are limited by a shortage of providers. This article looks at the impact of providing community-based depression treatment to low-income adults, and finds that it improves mental health and schooling outcomes for older children, and reduces risk tolerance. Additionally, pairing pharmacotherapy with livelihoods assistance provides additional benefits at a low additional cost.
Depression is a pervasive and costly illness with a lifetime prevalence of 15-20% (Kessler and Bromet 2013). It is the fourth largest contributor to the global burden of disease, and the third largest source of years lost to disability (James et al. 2018). Depression is more prevalent among the poor (Ridley et al. 2020) and may contribute to poverty and poverty traps.
For India and other developing countries, it is particularly important to understand the economic impact of depression, and to identify effective and scalable treatments. Although the Mental Health Care Act of 2017 creates a legally binding right to mental health care in India (Duffy and Kelly 2019), only 15% of people with depression in India receive care, since treatment options are limited by a shortage of providers (Saxena et al. 2007, Gautham et al. 2020).
Effectiveness of depression treatment
Psychotherapy and pharmacotherapy are the leading approaches to depression treatment. Psychotherapy typically involves regular extended interactions with a trained counselor or psychologist. Under pharmacotherapy, on the other hand, a psychiatrist treats the patient with antidepressants such as selective serotonin reuptake inhibitors (SSRIs). These drugs, which are manufactured generically in India, have been widely used for decades and have relatively mild side effects (Ferguson 2001, Cascade et al. 2009). Since it requires fewer personnel than psychotherapy, pharmacotherapy may be a valuable tool to treat depression in low- and middle-income countries (LMICs), where mental health specialists are scarce.
Evidence regarding the effectiveness of pharmacotherapy in low-income settings is limited (Patel et al. 2007). Clinical research from industrialised countries has demonstrated the effectiveness of pharmacotherapy (Gartlehner et al. 2017). However, we lack evidence of the effectiveness of community-based pharmacotherapy in LMICs, as well as knowledge of how and why mental health care may affect outcomes such as time use, earnings, and investment.
Our study
In a recent study (Angelucci and Bennett 2022), we evaluated the impacts of community-based pharmacotherapy in Karnataka.
We recruited 1,000 low-income adults (86% of whom were female) with mild or moderate depression symptoms in three peri-urban taluks near Bangalore. We provided pharmacotherapy and livelihoods assistance – such as support to find a new job or develop an income-generating activity – by cross-randomising each intervention, so that participants were offered either pharmacotherapy, livelihoods assistance, or both. The pharmacotherapy (PC) intervention provided eight months of personalised pharmacotherapy with the diagnosis and oversight of a psychiatrist from a local research hospital. In the initial visit, psychiatrists diagnosed patients, explained the significance of mental illness, and proposed an individualised course of treatment. Patients returned for monthly follow-up visits. The livelihoods assistance (LA) intervention involved two group meetings that discussed ways to earn income and deal with on-the-job challenges. Staff then helped participants pursue income-generating activities through job placements, small loans, or training, according to participants' individual circumstances. The PC/LA arm received both interventions, and a control arm did not receive either intervention.
Of the participants, 44% attended at least one psychiatric visit, and 68% attended at least one LA group or individual meeting. This level of take-up suggests that it is possible to surmount barriers to mental health treatment such as a lack of awareness and high stigma. We assessed impacts on depression and socioeconomic outcomes over 26 months, including the period while the PC intervention was ongoing and for over a year after PC had concluded. This duration of follow-up, which is unusual in mental health trials, enables us to judge both the short-term and long-term impacts of pharmacotherapy.
Effects of pharmacotherapy on mental health
We found that both the PC and PC/LA arms improved mental health. However, the combined PC/LA intervention had a significantly larger and more durable impact. Figure 1 shows the distribution of PHQ-9 scores1 by intervention arm while the PC intervention was ongoing (left panel) and up to 18 months after PC had concluded (right panel). PC/LA reduced depression severity by 0.26 standard deviations2 during the PC intervention, and by 0.24 standard deviations after the PC intervention. When offered alone, PC reduced depression severity by 0.14 standard deviations during the PC intervention and did not have a statistically significant effect afterward. LA alone had negligible effects on mental health. These estimates include individuals who complied with the interventions as well as those who did not (intent to treat effects)3. We expect that effects are roughly twice as large among participants who actually complied.
Figure 1. Distribution of depression severity by intervention arm, during (left panel) and after (right panel) the PC intervention
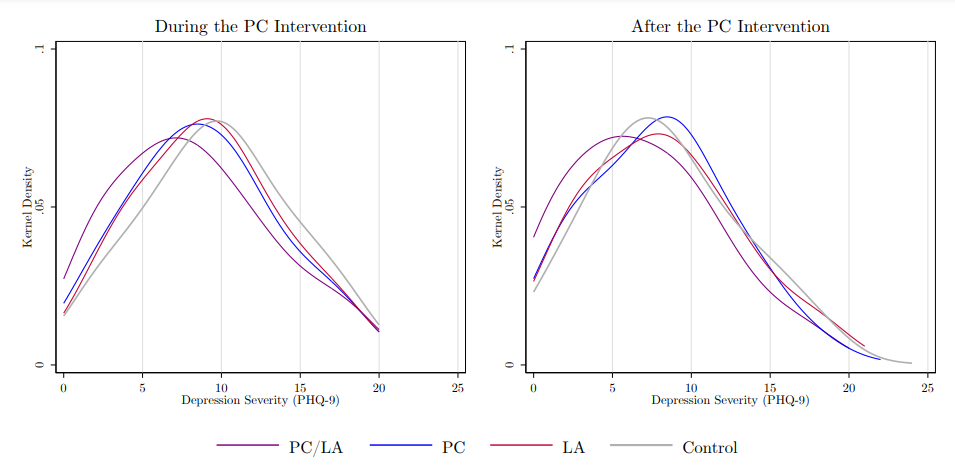
Note: A density plot is a visual representation of how the values of one variable, the PHQ-9 in this case, are distributed in our sample.
Effects of pharmacotherapy on work time or earnings
We did not find that PC increased work time or earnings. In fact, PC temporarily reduced work time by 5.4 hours per week and reduced earnings by Rs. 65 per week, a 10% decrease in both outcomes. The combined PC/LA intervention did not have these effects. Most of our study participants were women, and the lack of an improvement in these outcomes aligns with similar studies of mostly female samples in South Asia (Baranov et al. 2020, Bhat et al. 2022).
Effects of pharmacotherapy on human capital investment in children
We aggregated school enrollment, attendance, homework time, and (the lack of) labour force participation into a ‘child human capital investment’ index, and found that it was substantially impacted by PC, especially for older children, as Figure 2 illustrates. For children who were 12 or older (the age of transition to secondary school), PC increased human capital investment by around 0.4 standard deviations. These results were driven by large increases in enrollment and declines in labour force participation. We did not find effects for children aged 5-11, likely because most children of this age were already enrolled in school and did not work for pay.
Figure 2. Impacts on child human capital investment index after the PC intervention
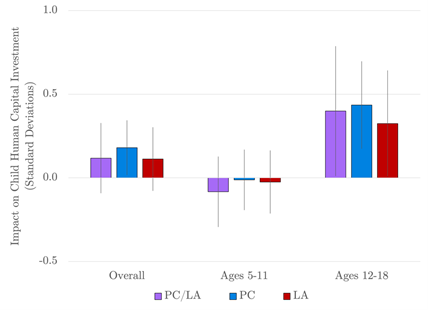
Note: Error bars show 90% confidence intervals. A 90% confidence interval means that if you were to repeat the experiment over and over with new samples, 90% of the time the calculated confidence interval would contain the true effect.
These effect sizes are comparable to the impacts of various educational interventions on enrollment, including conditional and unconditional cash transfers. This result suggests that the well-known correlation between parental depression and child development is at least partially causal. Therefore, adult mental health may be an important demand-side constraint on child human capital accumulation.
Effects of pharmacotherapy on risk tolerance and negative shocks
The interventions also made people less risk tolerant, although the timing and significance of the effects varied across arms. PC reduced risk tolerance by around 0.2 standard deviations after the conclusion of the intervention. We also measured whether households had recently experienced several negative shocks. If people are less tolerant of risk, they likely invest more in preventing negative shocks. Consistent with this hypothesis, we also found that PC reduced the incidence of negative shocks such as death, asset losses, or fire, by around 0.1 standard deviations.
The effect of PC on risk tolerance suggests that mental health may influence economic preferences. Anhedonia and pessimism are two primary depression symptoms that may lead people with depression to perceive less benefit from actions that improve their wellbeing. By alleviating these symptoms, pharmacotherapy could encourage investment to prevent negative shocks, as well as investment in children.
Effects of adding livelihoods assistance to pharmacotherapy
As described above, pairing PC with LA increased the size and duration of the positive impact on mental health. As an additional benefit, pairing PC with LA safeguarded against some transitory negative effects of PC: in the short run, PC reduced work time, activities of daily living (a health measure), and household consumption. We did not observe any of these effects in the arm that received both PC and LA. As implemented, LA added only 5% (Rs. 749) per participant to the intervention costs.
Future research should investigate the complementarity between PC and LA, and whether other inexpensive light-touch interventions could enhance the benefit of mental health care in a similar way. Since LA did not directly increase work time or earnings, features other than job-related benefits of LA may have impacted mental health. The group and individual social interactions that occurred under LA may have enabled participants to receive emotional support from like-minded peers. PC/LA participants also had better medication adherence, suggesting that LA could have improved their ability to plan or follow through. LA might have also helped participants overcome the stigma of receiving mental health care by supplying a reason for accepting mental health care.
Conclusion
There is an urgent need to identify effective and scalable ways to provide mental health care in India. Our findings suggest two pathways through which depression may contribute to poverty across generations: adult depression may reduce investment in child education; and make people more risk tolerant, exposing them to additional shocks that make it more difficult to escape poverty.
However, our trial suggests that community-based pharmacotherapy is feasible using local resources and may be a cost-effective way to treat depression in the community. Pairing pharmacotherapy with livelihoods assistance or other light-touch programmes may amplify the benefit of mental health treatment.
Notes:
- The PHQ-9 (Patient Health Questionnaire-9) objectifies and assesses the degree of depression severity through a questionnaire.
- Standard deviation is a measure that is used to quantify the amount of variation or dispersion of a set of values from the mean value (average) of that set.
- Intent to treat effects are based on an assessment of the people taking part in a trial, based on the group they were initially (and randomly) allocated to, and not the treatment they eventually received (that is, regardless of whether they dropped out, fully adhered to the treatment or switched to an alternative treatment).
Further Reading
- Angelucci, M and D Bennett (2022), ‘The Economic Impact of Depression Treatment in India: Evidence from Community-Based Provision of Pharmacotherapy,’ Unpublished manuscript. A version of this paper is available here.
- Bhat, B, et al. (2022), ‘The Long-Run Effects of Psychotherapy on Depression, Beliefs, and Preferences,’ NBER Working Paper 30011.
- Baranov, Victoria, Sonia Bhalotra, Pietro Biroli and Joanna Maselko (2020), “Maternal Depression, Women’s Empowerment, and Parental Investment: Evidence from a Randomized Controlled Trial,” American Economic Review, 110(3): 824-59.
- Cascade, Elisa, Amir H Kalali and Sidney H Kennedy (2009), “Real-World Data on SSRI Antidepressant Side Effects,” Psychiatry, 6(2). Available here.
- Duffy, Richard M and Brendan D Kelly (2019), “India’s Mental Healthcare Act, 2017: Content, Context, Controversy,” International Journal of Law and Psychiatry, 62: 169-178.
- Ferguson, James M (2001), “SSRI antidepressant medications: adverse effects and tolerability,” Primary Care Companion to the Journal of Clinical Psychiatry, 3(1).
- Gartlehner, Gerald, et al. (2017), “Pharmacological and non-pharmacological treatments for major depressive disorder: review of systematic reviews,” BMJ Open, 7(6): e014912. Available here.
- Gautham, Melur Sukumar, et al. (2020) “The National Mental Health Survey of India (2016): Prevalence, socio-demographic correlates and treatment gap of mental morbidity,” International Journal of Social Psychiatry, 66(4): 361-372.
- James, Spencer L, et al. (2018), “Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017,” The Lancet, 392(10159): 1789-1858.
- Kessler, Ronald C and Evelyn J Bromet (2013), “The epidemiology of depression across cultures,” Annual Review of Public Health, 34: 119-138.
- Patel, Vikram, et al. (2007), “Treatment and prevention of mental disorders in low-income and middle-income countries,” The Lancet, 370(9591): 991-1005.
- Ridley, Matthew, Gautam Rao, Frank Schilbach, and Vikram Patel (2020), “Poverty, depression, and anxiety: Causal evidence and mechanisms”, Science, 370(6522).
- Saxena, Shekhar, Graham Thornicroft, Martin Knapp and Harvey Whiteford (2007), “Resources for mental health: scarcity, inequity, and inefficiency,” The Lancet, 370(9590): 878-889.




 23 August, 2022
23 August, 2022 





Comments will be held for moderation. Your contact information will not be made public.