Private health insurance covering tertiary diseases is limited to the upper middle class in India. One reason for low take-up of publicly-financed health insurance among economically weaker sections is that treatment of tertiary diseases relies critically on specific information on facilities and treatment options. This column presents evidence from Andhra’s Aarogyasri programme suggesting that community networks might be an important channel through which such information is obtained.
Apart from the quality of life and income, poor health affects the well-being of families socially and psychologically. The economic burden of bad health is tangible and substantial. For example, out-of-pocket expenditures on treatment and services for HIV/AIDS and antiretroviral treatment in India in 2005 were reported at Rs. 6,000 (US$90 approx.) and Rs. 18,150 per person (US$275 approx.) respectively, for a six-month reference period (Burden of Disease in India, 2005). Roughly 40% to 70% of these expenditures are financed by borrowing or selling assets. Approximately one-third of households in India face catastrophic healthcare expenditures where out-of-pocket payments exceed the household’s ability to pay by 40% (Raban et al. 2013). For poorer households, catastrophic healthcare expenditure followed by temporary or permanent job loss may effectively lead to impoverishment. Indeed, research estimates that catastrophic healthcare expenditures are associated with 2.7 percentage points increase in extreme poverty in Asia (van Doorslaer et al. 2006).
The burden of disease
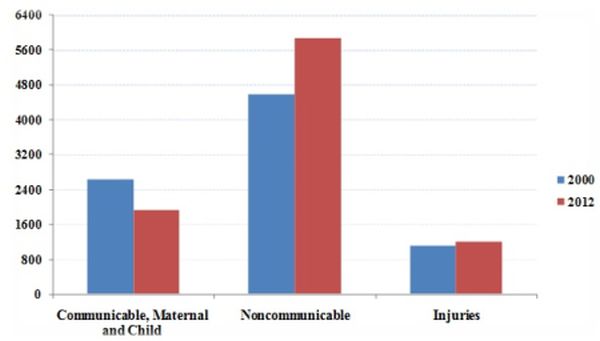
Communicable diseases, and maternal and child health conditions account for nearly half of India’s disease burden. Healthcare policies focus primarily on communicable diseases as they pose large negative externalities to society and are usually less resource intensive to address. As a result, the incidence of communicable diseases, such as malaria, tuberculosis, diarrhoea has reduced sharply, and polio and leprosy have almost been eliminated. The number of deaths from communicable diseases has decreased from 2.6 million in 2000 to 1.9 million in 2012 (Department of Health Statistics and Information Systems, World Health Organization (WHO), 2014). Meanwhile, non-communicable, tertiary diseases in India and elsewhere in South Asia have increased disproportionately (Figure 1) but received relatively less attention from policymakers.
Figure 1. Distribution of burden of disease in India and South Asia over time
Panel A. India
Panel B. South Asia
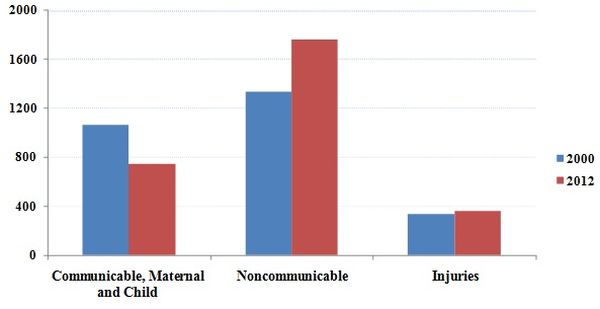 Source: Data from Global Health Estimates 2104 Summary Tables, World Health Organization (WHO).
Source: Data from Global Health Estimates 2104 Summary Tables, World Health Organization (WHO). Notes: (i) South Asian countries include Afghanistan, Bangladesh, Bhutan, Myanmar, Nepal, Pakistan and Sri Lanka. (ii) The vertical axes represent number of deaths in 1,000.
India’s public interventions toward tertiary diseases are mostly limited to subsidised healthcare services through facilities that are directly owned and operated by the government. In practice, the vast majority of these public healthcare facilities have poor quality and often crowd out private healthcare providers.
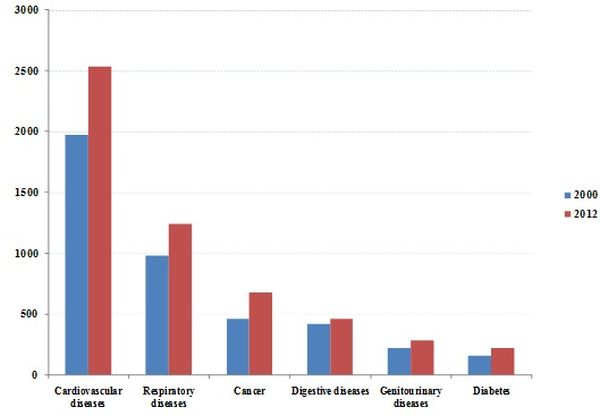
The treatment of tertiary diseases such as cancer, diabetes, cardiovascular and respiratory diseases require better facilities. Additionally, recent trends suggest that the burden of such disease is slated to increase fairly sharply while incidents of deaths from communicable diseases are declining.
Figure 2. Burden of tertiary diseases in India over time
Health insurance coverage
Insurance against catastrophic health expenditure may increase the ability of economically weaker households to save and invest their way out of poverty. In many developed nations, where insurance markets are developed, health insurance coverage is almost universal. However, in the context of developing countries, despite being heavily subsidised, health insurance coverage is negligible. In India, 86% of all health expenditure is out of pocket, with only 15% of Indian households reporting any insurance coverage (WHO, 2011). Utilisation of Rashtriya Swasthya Bima Yojna (RSBY), a central government-operated health insurance programme providing insurance coverage to Below Poverty Line (BPL) households in 25 states, is between 11% and 55% in the district of Amravati in Maharashtra (Rathi et al. 2012) and “virtually zero” in the state of Karnataka (Rajasekhar et al. 2011).
One reason why the private market fails is because only the chronically unhealthy try to enrol, so the premiums quickly spiral beyond affordability. Another reason might be that poor households do not understand the benefits of health insurance. Finally, households may not trust insurance providers to reimburse claims, especially since few private firms have good track records in processing and paying claims. Indeed, commenting on the participation of the poor in financial inclusion schemes, N. C. Saxena, a former member of the erstwhile National Advisory Council, said “Typically, people in that strata of society are circumspect about any scheme, which needs them to put in money - simply because they do not trust that they will get this money back.” (Nair 2016).
Publicly-funded programmes with cashless transactions and no co-payments or deductibles might have the potential to increase adoption of health insurance. If premiums are paid directly by the government, trust in the provider or liquidity constraints in paying premiums are not significant barriers to take-up. If coverage is automatic or universal, then understanding programme details is not necessary for eligible populations to obtain insurance.
Even so, the treatment of tertiary diseases relies critically on information about which specialty hospitals and physicians provide the best care, treatment options, as well as information on how to use the programme. Peers and social networks might be an important channel through which such information is obtained. Our research - focusing on the context of Aarogyasri, a public health insurance programme in Andhra Pradesh and Telangana - explores to what extent caste and gender networks affect the utilisation of publicly-financed health insurance for tertiary care (Debnath, Jain and Singh 2015).
Andhra’s Aarogyasri programme
Aarogyasri is a cashless health insurance programme for BPL households in Andhra Pradesh (and Telangana since the state’s formation in 2014). The programme covers medical bills up to Rs. 200,000 (US$3,000 approx.) for the treatment of serious ailments such as cancer, kidney failure, heart and neurosurgical disease that require hospitalisation. All transactions are cashless where beneficiaries can go to any authorised hospital and receive care without paying upfront for the covered procedures. The insurance does not have any deductible or co-payment. The programme is operated by the Aarogyasri Health Care Trust and managed by a private insurance company. Currently, 938 treatments are covered under the programme. Almost 90% of the population of the two states possesses a BPL card making the programme almost universal. As of December 2013, about 2.1 million procedures have been performed under the programme with more than US$800 million claimed cumulatively by beneficiaries.
Figure 3. Aarogyasri utilisation over time
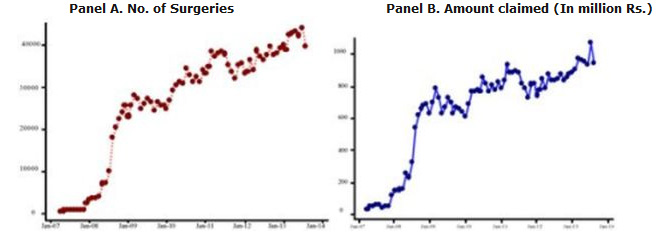 Note: Data consists of all claims filed under the public health insurance programme Aarogyasri for the period 2008-2013.
Note: Data consists of all claims filed under the public health insurance programme Aarogyasri for the period 2008-2013.
As of May 2014, 663 public or private hospital hospitals were empanelled under Aarogyasri. The Aarogyasri Trust pays healthcare providers on a case-by-case basis at a predefined rate. Hospitals conduct free health camps for patients and help desks facilitate patient access at primary health centres, area/district hospitals and network hospitals.
Learning through community networks
Our analysis of the Aarogyasri programme suggests that members of the same caste in the same village are important sources of programme information. In particular, if caste peers use Aarogyasri in the previous quarter, then an individual is 19% more likely to claim Aarogyasri benefits for the first time. Interestingly, other caste groups within the same village and the same caste members in other nearby villages have virtually no effect on utilisation. This finding is consistent with healthcare decisions being localised, with immediate family and friends as the central sources of information.
We also find that a range of other factors are complementary to community networks. For example, caste network effects are stronger in urban areas and in regions with greater penetration of cell phones and radios. These imply that proximity to peers, or at least the ability to contact them quickly, greatly facilitates the effectiveness of social networks in providing programme information.
Networks might be ineffective in disseminating information for diseases that require patients to reveal private and sensitive information to their friends. Conversely, some diseases such as cancer are informationally intense to treat, and patients need the advice of their friends and relatives to make treatment decisions. Our results show that network effects are the largest for cardiology, nephrology and urinary surgery, with oncology and paediatrics patients also relying extensively on their peers. In contrast, network effects associated with ophthalmology, plastic surgery and dermatology, and gastroenterology are lower, perhaps because decision-making by patients is less complex for these procedures.
These findings have implications for strategies to improve the treatment of tertiary diseases in India and other developing countries. By uncovering the role of community networks on healthcare use, our findings suggest that welfare programmes should incorporate network-based learning, in addition to direct information provision, to increase participation. This approach has been tried, for instance in the case of Mahadalits1 in Bihar with positive results (Kumar and Somanathan 2015). Specifically, for publicly-financed health insurance, researchers also find that community liaisons are effective in encouraging enrolment in RSBY (Berg et al. 2013). Future research, with a sharper focus on implementation, could help understand and operationalise the network-based approach to increasing healthcare use.
Notes:
- Dalit, meaning ‘oppressed’, is a term of pride used by formerly untouchable castes, lowest in the caste hierarchy, officially known as Scheduled Castes. The poorest Dalits have been declared Mahadalits in the state of Bihar.
Further Reading
- Berg, E, M Ghatak, R Manjula, D Rajasekhar and S Roy (2013), ‘Motivating knowledge agents: Can incentive pay overcome social distance?’, CEPR Discussion Paper No. DP9477. Available at: http://personal.lse.ac.uk/ghatak/agentincentives.pdf
- Currie, Janet and Jonathan Gruber (1996), “Health insurance eligibility, utilization of medical care, and child health”, Quarterly Journal of Economics, 111(2): 431-466. Available at: http://www.nber.org/papers/w5052.pdf.
- Debnath, S, T Jain and M Singh (2015), ‘Social networks and health insurance utilization’, Indian School of Business, Working Paper. Available at: http://www.isid.ac.in/~epu/acegd2015/papers/TarunJain.pdf.
- Kumar, H and R Somanathan (2015), ‘Caste connections and government transfers: The Mahadalits of Bihar’, Delhi School of Economics, Working Paper. Available at: http://www.isid.ac.in/~epu/acegd2015/papers/HemanshuKumar.pdf.
- Nair, R (2016), ‘Flagship government schemes set for a revamp’, Mint, 25 January 2016.
- National Commission on Macroeconomics and Health (2005), ‘Burden of Disease in India’, Background Papers, Ministry of Health and Family Welfare, Government of India, New Delhi, September.
- Raban, Magdalena, Rakhi Dandona and Lalit Dandona (2013), “Variations in catastrophic health expenditure estimates from household surveys in India", Bulletin of the World Health Organization 91(10): 726-735.
- Rajasekhar, D, Erlend Berg, Maitreesh Ghatak, R Manjula, and Sanchari Roy (2011), “Implementing health insurance: The rollout of Rashtriya Swasthya Bima Yojana in Karnataka”, Economic and Political Weekly 46(20): 56-63. Available at: http://personal.lse.ac.uk/ghatak/RSBY%20EPW.pdf
- Prateek, Rathi, Arnab Mukherji and Gita Sen (2012) “RSBY: Evaluating Utilization, Roll-out and Perceptions in Amaravati District”, Economic and Political Weekly, Special Articles, 57-64.
- van Doorslaer, Eddy, Owen O´Donnell, Ravi Rannan-Eliya, Aparna Somanathan, Shiva Raj Adhikari, Charu Garg and Deni Harbianto (2006), “Effect of payments for health care on poverty estimates in 11 countries in Asia: An analysis of household survey data”, The Lancet 368(9544): 1357-1364.
- WHO (2014), ‘Estimates for 2000-2012’, Department of Health Statistics and Information Systems, World Health Organization.




 12 April, 2016
12 April, 2016 




Comments will be held for moderation. Your contact information will not be made public.