Groundwater contaminated with arsenic is a serious public health threat in rural India. This column presents results from a field experiment conducted in Bihar to assess the demand for fee-based testing of wells for arsenic, and to study the behavioural responses of households to well-specific arsenic information.
Information regarding environmental quality can help in reducing the health burden of environmental shocks by encouraging avoidance. This is particularly important in developing countries, where willingness to pay for information on environmental quality is low, while environmental monitoring is weak. On the other hand, adverse environmental quality may affect economic development through the health and productivity channels. So, it is important to understand the demand for information about local environmental quality risks and how people respond to such information (Pattanayak et al. 2009, Somanathan 2010, Greenstone and Jack 2015).
Arsenic in groundwater
Well testing for arsenic is a case where access to information about environmental quality can facilitate low-cost avoidance and preventive measures. A well that meets guidelines for arsenic in drinking water may be found in immediate neighbourhood of a very unsafe well. Arsenic contamination can vary greatly over small distances throughout the affected portions of the Indo-Gangetic Plain in Bangladesh, India, and Pakistan, but does not vary much over time (van Geen et al. 2013). Well tests therefore provide an effective way to avoid exposure, namely by switching to a nearby safe well (van Geen et al. 2002, Ahmed et al. 2006). Much like other basic preventive health products, arsenic tests are very cost efficient. The cost of the kit itself is on the order of only US$ 0.35 per test (about Rs. 25) although the total cost of goods and services including the placard showing contamination level reaches up to US$ 2.26 (about Rs. 150). Testing wells for arsenic provides information that is not substitutable because the distribution of arsenic in groundwater is difficult to predict.
On the other hand, the health consequences of chronic arsenic exposure are dramatic. Flannagan et al. (2012) concluded on the basis of two separate cohort studies that high arsenic exposure was responsible for over 5% of mortality in Bangladesh. Arsenic in tubewell water has also been associated with impaired intellectual and motor function in children (Wasserman et al. 2004, Parvez et al. 2011). In consequence, there are significant effects on income and labour supply: Pitt et al. (2015) estimate that lowering the amount of retained arsenic among adult men in Bangladesh to levels encountered in uncontaminated countries would increase earnings by 9%. Matching households to arsenic exposure, Carson et al. (2011) found that overall household labour supply is 8% smaller due to arsenic exposure. Chowdhury et al. (2015) estimate that the mental health burden of arsenic contamination for affected individuals alone can be as high as the average annual household income in Bangladesh.
Study of fee-based well testing
Because of their low cost, important health benefits, and absence of private provision, arsenic well tests have been provided in some areas free of charge through public provision. However, such programmes have not come close to comprehensively covering the geographic area where arsenic is of concern, including in our study area. In addition, any one-time public provision becomes ineffective when wells continue to be installed in previously-tested areas. Most wells installed since a massive blanket testing campaign of five million wells in Bangladesh which ended in 2005, for instance, have never been tested for arsenic (van Geen et al. 2014).
Our study explores the possibility of selling tests as a way of increasing coverage beyond what has been achieved by public provision. The underlying motivation is that a cost-shared private provision could create market for arsenic tests in which local entrepreneurs would have an incentive to seek out untested wells. For this study of fee-based arsenic testing, supported in part by IGC (International Growth Centre) India Central, a randomised controlled trial was conducted in 26 villages in Bihar, India, from 2012-2015 (Table 1). In order to elicit demand, we offered tests at prices between Rs. 10 to Rs. 50, randomised at the village level (Figure 1). The highest price level (Rs. 50) – one-third of the full cost of goods and services – was slightly less than one day of per capita income in Bhojpur district in 2011-12.
Table 1. Timeline of the field experiment
| August 2012 | Arsenic testing in pilot villages |
| November 2012 – February 2013 | First round of arsenic testing |
| February 2013 – May 2013 | Follow-up survey of well switching |
| November 2014 – January 2015 | Second round of arsenic testing |
Figure 1. Map of study area in Bihar showing the outcome of testing in the form of pie diagrams
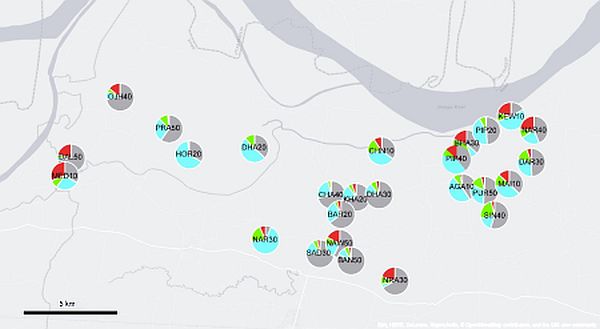
Note: Map shows test outcomes in 26 villages. The price charged in Rs. for tests is indicated by the last two digits of each label. The grey, blue, green, and red sections of each pie indicate no test result, <10, 10-50, and >50 microgram arsenic per litre, respectively.
Demand for arsenic testing
We found that there is a considerable demand for arsenic testing: on average across price groups, and over the duration of our intervention, 45% of households purchase the test (Figure 2). However, demand drops steeply with price, in line with demand elasticities found in other studies of highly effective preventive healthcare products (Cohen and Dupas 2010, Kremer and Miguel 2007). We repeat the sales offer two years after the initial campaign, at the same (nominal) sales price and record additional demand, with overall coverage rising from 27% to 45%1. We find little evidence on wealthier household purchasing more tests at higher prices. We also test if high-contamination well owners were more or less likely to pay higher price but find no supporting evidence, which suggests that households themselves were unable to predict arsenic level in their water well correctly.
Figure 2. Price sensitivity to demand for arsenic tests
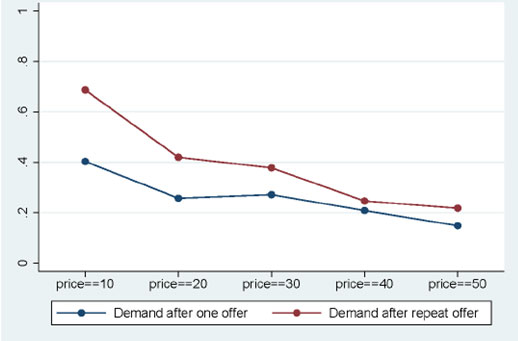
Note: The plot shows demand patterns after one offer (2012) and after two offers. 2012 demand estimates are obtained from recall of sales offers and purchases as measured in the 2014 survey.
Household response to information on environmental quality
We further investigate how households respond to the information on environmental quality. Test results indicate only one out of every two wells is safe – about 19% wells have high arsenic (that is, more than 50 microgram arsenic per litre) and next 31% wells are also moderately contaminated. In a follow-up survey to measure behavioural responses of households (conducted three months after the first wave of test offers), we find about one-third of households whose wells had unsafe levels of arsenic reported having switched to a safer tube well for their drinking and cooking water needs2,3. Evidence on significant switching in response to subsidised diagnostic test for arsenic stands in contrast to limited evidence on behavioural responses (that is, seeking malaria treatment) to the information provided by subsidised diagnostic test for malaria in Kenya (Cohen et al. 2015). We find no effect of price paid for testing on the probability of switching to safer water sources, which is an important finding in assessing cost and benefit of programmes that provide information on environmental quality. The cost of switching should depend on the distance to a safer well, and we indeed find that probability of switching is negatively correlated to such distance (Figure 3).
Figure 3. Well switching and distance to safe well
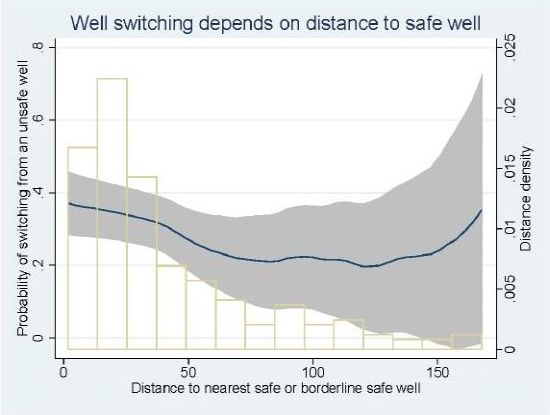
Note: The graph shows the probability that household whose wells tested ‘red’ (high arsenic) in 2012 switched to a safer (‘blue’ or ‘green’) well, conditional on distance (in metres) to the nearest safer well.
In a novel finding, we find strong evidence of selective recall and concealing of test results. About half of the households whose wells tested unsafe were unable to recall their well status correctly (with no significant difference in case of safe wells). We also document that households actively conceal information on their well’s arsenic level when tests revealed their well water to be high in arsenic, by discarding placards attached to high-arsenic wells. Stigma, concerns over reduced property value, or obstacles to switching might explain this choice. We present evidence that wealthier households are more likely to hide adverse information.
Policy implications
The demand for arsenic tests documented in Bihar is consistent with other studies of cost-sharing in basic preventive healthcare products. Because demand is greatly affected by the extent of cost-sharing, the role of a large subsidy is critical for ensuring maximum coverage. A new key finding is that a repeat offer made within two years met with significant demand. This underscores the need for a more careful assessment of experimental evidence generated with one-time offers, or offers available only for a short period. Given selective recall, the question of how best to provide information to households in a way that is salient but not socially or privately costly deserves additional attention.
In India, there is an urgent need to carry out arsenic testing in all affected areas, followed by provision of safe drinking water. We document that arsenic contamination affects about half of private, drinking-water wells in our study area in rural Bihar. While supplying treated water with pipelines is an obvious solution, expanding access in rural areas will be costly and will require time. Recent Union Budget for 2017-18 mentions increasing access of piped water to 28,000 arsenic and fluoride affected habitations under the National Rural Drinking Water Programme in next four years, with an average allocation of about Rs. 9 million per habitation. Given the scale and implications of continued use of arsenic contaminated water, a broader programme needs to be in place to provide information on the water quality of private wells, with a subsidised testing campaign in rural areas. Further research can help identify ways to encourage sharing of safe drinking water among nearby households.
Notes:
- The demand is somewhat lower than previously reported by van Geen and Singh (2013) because we learned since that enumerators did not systematically collect data from all households approached with a sales offer. We therefore used recall data on sales offers and purchases during the second offer phase for a better estimate of demand during the first phase.
- This avoidance rate is in line with previously reported switching rates, though at the lower end of the spectrum (Ahmed et al. 2006, Bennear et al. 2013, Chen et al. 2007, George et al. 2012a, Madajewicz et al. 2007, Opar et al. 2007).
- We find almost negligible switching from safe wells to other wells.
Further Reading
- Ahmed, M Feroze, Satinder Ahuja, Mohammad Alauddin, Stephan J Hug, Jon R Lloyd, Alex Pfaff, Thomas Pichler, Chad Saltikov, Martin Stute, and Alexander van Geen (2006), “Ensuring safe drinking water in Bangladesh”, Science, 314(5806):1687-1688. Available here.
- Barnwal, P, A van Geen, J von der Goltz and CK Singh (2017), ‘Demand for environmental quality information and households´ response: Evidence from well-water arsenic testing’, India, Mimeo.
- Bennear, Lori, Alessandro Tarozzi, Alexander Pfaff, Soumya Balasubramanya, Kazi Matin Ahmed, and Alexander van Geen (2013), “Impact of a randomized controlled trial in arsenic risk communication on household water-source choices in Bangladesh”, Journal of Environmental Economics and Management, 65(2):225–240. Available here.
- Carson, Richard T, Phoebe Koundouri and Celine Nauges (2011), “Arsenic mitigation in Bangladesh: A household labor market approach”, American Journal of Agricultural Economics, 93:407-414. Available here.
- Chen, Yu, Alexander van Geen, Joseph H Graziano, Alexander Pfaff, Malgosia Madajewicz, Faruque Parvez, A Iftekhar Hussain, Vesna Slavkovich, Tariqul Islam and Habibul Ahsan (2007), “Reduction in urinary arsenic levels in response to arsenic mitigation efforts in Araihazar, Bangladesh”, Environmental Health Perspectives, 115(6):917–923. Available here.
- Chowdhury, S, A Krause and KF Zimmermann (2015), ‘Arsenic contamination of drinking water and mental health’, CEPR Discussion Paper No. DP10978. Available here.
- Cohen, Jessica and Pascaline Dupas (2010), “Free distribution or cost-sharing? Evidence from a randomized malaria prevention experiment”, The Quarterly Journal of Economics, 125(1):1–45. Available here.
- Cohen, Jessica, Pascaline Dupas and Simone Schaner (2015), “Price subsidies, diagnostic tests, and targeting of malaria treatment: evidence from a randomized controlled trial”, The American Economic Review, 105(2):609–645. Available here.
- Dupas, Pascaline (2014), “Getting essential health products to their end users: Subsidize, but how much?”, Science, 345:1279-1281.
- Flanagan, Sara V, Richard B Johnston and Yan Zheng (2012), “Arsenic in tube well water in Bangladesh: health and economic impacts and implications for arsenic mitigation”, Bulletin of the World Health Organization, 90:839-46.
- George, Christine Marie, Alexander van Geen, Vesna Slavkovich, Ashit Singha, Diane Levy, Tariqul Islam, Kazi Matin Ahmed, Joyce Moon-Howard, Alessandro Tarozzi, Xinhua Liu, Pam Factor-Litvak and Joseph Graziano (2012a), “A cluster-based randomized controlled trial promoting community participation in arsenic mitigation efforts in Bangladesh”, Environmental Health, 11(1):1–10.
- Greenstone, Michael and B Kelsey Jack (2015), “Envirodevonomics: A research agenda for an emerging field”, Journal of Economic Literature, 53(1):5–42. Available here.
- Kremer, Michael and Edward Miguel (2007), “The illusion of sustainability”, The Quarterly Journal of Economics, 122:1007-1065. Available here.
- Madajewicz, Malgosia, Alexander Pfaff, Alexander van Geen, Joseph Graziano, Iftikhar Hussein, Hasina Momotaj, Roksana Sylvi, and Habibul Ahsan (2007), “Can information alone change behavior? Response to arsenic contamination of groundwater in Bangladesh”, Journal of Development Economics, 84:731–754. Available here.
- Opar, Alisa, Alex Pfaff, A Seddique, K Ahmed, Joseph Graziano and Alexander van Geen (2007), “Responses of 6,500 households to arsenic mitigation in Araihazar, Bangladesh”, Health & Place, 13(1):164–172. Available here.
- Parvez, Faruque, Gail A Wasserman, Pam Factor-Litvak, Xinhua Liu, Vesna Slavkovich, Abu B Siddique, Rebeka Sultana, Ruksana Sultana, Tariqul Islam, Diane Levy, Jacob L Mey, Alexander van Geen, Khalid M Khan, Jennie Kline, Habibul Ahsan and Joseph H Graziano (2011), “Arsenic exposure and motor function among children in Bangladesh”, Environmental Health Perspectives, 119:1665-1670. Available here.
- Pattanayak, Subhrendu K and Alex Pfaff (2009), “Behavior, environment, and health in developing countries: evaluation and valuation”, Annual Review of Resource Economics, 1(1):183–217. Available here.
- Pitt, M, MR Rosenzweig and N Hassan (2015), ‘Identifying the hidden costs of a public health success: arsenic well water contamination and productivity in Bangladesh’, NBER (National Bureau of Economic Research), Working Paper w21741.
- Somanathan, Easwaran (2010), “Effects of information on environmental quality in developing countries”, Review of Environmental Economics and Policy, 4(2):275–292.
- van Geen, Alexander, Habibul Ahsan, Allen Horneman, Ratan K Dhar, Yan Zheng, Iftikhkar Hussain, Kazi Matin Ahmed, Andrew Gelman, Martin Stute, H James Simpson, Sean Wallace, Christopher Small, Faruque Parvez, Vesna Slavkovich, Nancy Lolacono, Marck Becker, Zhongqi Cheng, Hassina Momotaj, Mohammad Shahnewaz, Ashraf Ali Seddique and Joseph H Graziano (2002), “Promotion of well-switching to mitigate the current arsenic crisis in Bangladesh”, Bulletin of the World Health Organization, 80:732-737.
- van Geen, Alexander, Ershad B Ahmed, Lynnette Pitcher, Jacob L Mey, Habibul Ahsan, Joseph Graziano and Kazi Matin Ahmed (2014), “Comparison of two blanket surveys of arsenic in tubewells conducted 12 years apart in a 25km2 area of Bangladesh”, Science of the Total Environment, 488:484-492. Available here.
- van Geen, Alexander, Benjamin Bostick, Pham Thi Kim Trang, Vi Mai Lan, Nguyen-Ngoc Mai , Phu Dao Manh, Pham Hung Viet, Kathleen Radloff, Zahid Aziz, Jacob L Mey, Mason O Stah, Charles F Harvey, Peter Oates, Beth Weinman, Caroline Stengel, Felix Frei, Rolf Kipfer and Michael Berg (2013), “Retardation of arsenic transport through a Pleistocene aquifer”, Nature, 501(7466):204-207. Available here.
- van Geen, A and CK Singh (2013), ‘Piloting a novel delivery mechanism of a critical public health service in India: arsenic testing of tubewell water in the field for a fee’, IGC Policy Note 13/0238.
- van Geen, A and CK Singh (2013), ‘Reducing poisoning by arsenic in tubewell water’, Ideas for India, 11 March 2013.
- Wasserman, Gail A, Xinhua Liu, Faruque Parvez, Habibul Ahsan, Pam Factor-Litvak, Alexander van Geen, Zhongqi Cheng, Vesna Slavkovich, Iftikhar Hussain, Hassina Momotaj and Joseph H Graziano (2004), “Water arsenic exposure and children’s intellectual function in Araihazar, Bangladesh”, Environmental Health Perspectives, 112(17):1329-1333. Available here.




 20 February, 2017
20 February, 2017 






Comments will be held for moderation. Your contact information will not be made public.