Various studies have noted that vast inequalities – economic and socio-demographic – exist in maternal, newborn, and child health outcomes and utilisation of care services. In this post, Sohini Paul explores how inequality in the use of these services changed in the 10 years following the launch of the National Rural Health Mission in 2005. While service utilisation by the poor increased and the rich-poor gap declined in this period, coverage remains low among the poor and inequality persists.
India has, undeniably, made significant progress in improving the maternal, newborn, and child health (MNCH) situation over the past decades. However, the country is yet to reach the targets set for MNCH outcomes in national policies and international conventions. For example, although the maternal mortality ratio has declined from 301 per 100,000 live births in 2001-03 to 130 in 2014-16, India is yet to achieve the National Population Policy’s goal of reducing the figure to 100 by 2010, or the Millennium Development Goal of 109 by 2015.
Earlier studies have noted that wide inequalities – economic and socio-demographic – exist in MNCH outcomes and utilisation of MNCH services (Jejeebhoy and Santhya 2014, Paul et al. 2011). An analysis of who benefitted most from improvements in MNCH care services during 1992-2006, covered by first three rounds of the National Family Health Survey (NFHS), suggests that increments in antenatal care and skilled attendance at delivery were more likely to have been experienced by non-poor than poor mothers (Pathak, Singh, Subramanian 2010).
To improve the scenario, the Indian government implemented the National Rural Health Mission (NRHM) in 2005 with the intention of providing accessible, affordable, accountable, and good quality health services to all, especially to the poorest and those in the most remote areas of the country (Ministry of Health and Family Welfare, 2005). Under NRHM, Janani Suraksha Yojana, a conditional cash transfer scheme aimed at encouraging institutional delivery, was introduced; and Accredited Social Health Activists (ASHAs) were involved to serve as a link between the community and the public health system. The programme also emphasised the need for upgrading and strengthening facilities and infrastructure and skilling of healthcare providers. The NRHM was subsequently restructured as the National Health Mission (NHM) in 2013, to address the health needs of the urban population as well. Furthermore, under the national Reproductive, Maternal, Newborn, Child Health + Adolescent (RMNCH+A) initiative, a continuum of care model has been proposed that focuses on the pre-pregnancy stage shortly after marriage, and extends to the child care phase of the life cycle (MOHFW, 2013).
In this post, I analyse the extent to which the use of MNCH care services has improved among the poorest and the richest women in India, the extent to which economic inequalities in access to MNCH services have reduced or increased over time, and which components of MNCH care remain least and most equitable since the launch of NRHM in 2005 (Paul 2018).
Data and methodology
I use data from the 3rd and 4th rounds of NFHS conducted in 2005-06 and 2015-16 respectively. I compare MNCH care-seeking practices among the poorest women (that is, those who belonged to the bottom wealth quintile) and the richest women (that is, those who belonged to the topmost wealth quintile). My analysis focuses on MNCH care-seeking for the last birth among married women aged 15-49 who had given birth in the five years before the survey.
Outcome variables included the key components of care spanning over three stages of the continuum of care in maternal health: antenatal care, care during child delivery, and postnatal care. I estimate the average coverage of women who: (i) had their first antenatal check-up in the first trimester; (ii) received four or more antenatal check-ups; (iii) received at least two tetanus toxoid (TT2) injections; (iv) consumed iron and folic acid supplements (IFA) for at least 100 days; (v) underwent the following check-ups and tests at least once during antenatal visits – weight, blood pressure, blood test, urine test, and abdominal examination;(vi) had an institutional delivery; (vii) had skilled birth attendance during delivery; and (viii) received a health check-up within 48 hours of delivery.
I assess the evolution of inequality in utilisation of MNCH services between 2005-06 and 2015-16 by using Concentration Index (CI), a commonly used measure capturing relative inequality. CI quantifies the extent to which a health service coverage indicator is concentrated among the poorest or the richest.
Utilisation of MNCH care services
A comparison of the coverage of MNCH services in 2005-06 and 2015-16 shows that their utilisation has increased significantly since the launch of NRHM, regardless of the indicator used (Figure 1). However, the magnitude of improvements in coverage varies widely across indicators. For example, the highest increases over this period were observed for institutional delivery (from 41% to 81%), skilled birth attendance (50% to 83%), post-partum checkup within two days of delivery (36% to 65%), and receiving comprehensive tests and check-ups at least once during antenatal visits (35% to 64%). In comparison, the smallest increases were experienced for receiving two doses of TT injections (76% to 83%), at least four antenatal check-ups (37% to 51%), first check-up in the first trimester (44% to 58%), and consumption of IFA supplements for at least 100 days (15% to 30%).
Figure 1. Coverage of MNCH care services (%)
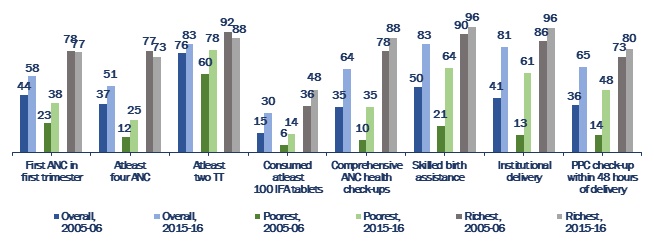 Note: Change in coverage between 2005-06 and 2015-16 was statistically significant for all indicators and all the three groups, except for the difference in the proportion of women who belonged to the wealthiest quintile and received their first antenatal check-up in the first trimester.
Note: Change in coverage between 2005-06 and 2015-16 was statistically significant for all indicators and all the three groups, except for the difference in the proportion of women who belonged to the wealthiest quintile and received their first antenatal check-up in the first trimester. Coverage increased significantly among poorest women, regardless of the indicator. However, the magnitude of improvements was larger among the poorest than among the richest, which is understandable given the low initial coverage of these indicators among the former. The analysis also reveals that despite greater improvement increase among the poorest, the level of health care services utilisation among them in 2015-16 remained far below that of the wealthiest in 2005-06.
Inequality in utilisation of MNCH care services
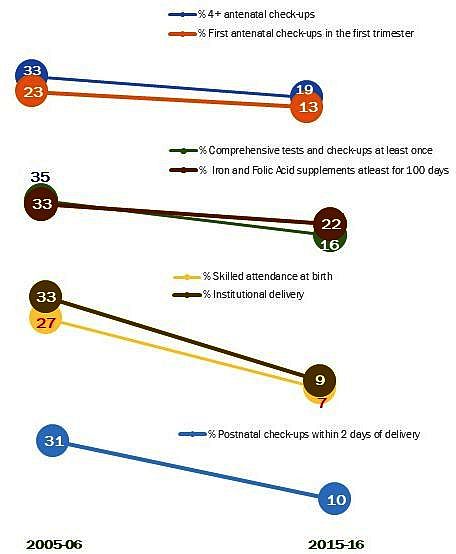
Inequality in utilisation of MCH services by household wealth status had reduced during 2006 and 2016 for all the indicators of MNCH care service coverage though magnitude of decline varies widely. In Figure 2, I present relative inequality in terms of CI*100. The largest decline in inequality was observed for institutional delivery, followed by skilled assistance during child birth, postnatal checkup within two days of child delivery, and receipt of comprehensive check-ups at least once during antenatal visits. On the contrary, the smallest decline was experienced for receipt of fist checkup in first trimester, followed by consumption of IFA supplements for at least 100 days, and four or more antenatal care visits during pregnancy.
Figure 2. Inequality in MNCH care services
Despite decline in inequality during the inter-survey period, findings show that inequality persists. The indicator that becomes the most equitable is receipt of two doses of TT2 injections in 2015-16. This is followed by skilled birth attendance and institutional delivery. The indicators for which there was least reduction in inequality include consumption of IFA supplements for at least 100 days, receipt of four or more antenatal check-ups, and receipt of comprehensive health check-ups at least once during antenatal visits, and receipt of first check-up in the first trimester.
Discussion and conclusions
In summary, I find that the coverage of MNCH care services has improved significantly across all indicators, particularly among the poorest. Even so, the coverage of several indicators remains low among the poorest section, especially those related to antenatal care. Furthermore, no more than 61-64% of the poorest women had institutional delivery and skilled birth attendance, despite the coverage of these indicators increasing dramatically at the national level. Likewise, although inequality in coverage of MCH indicators had declined, inequality still persists.
These findings call for further policy attention on MNCH care services for the poor. Interventions such as information campaigns using interpersonal channels and mass media, incentivising comprehensive antenatal care-seeking, increasing the number of frontline workers and lower-level facilities in areas that are most in need, task-shifting and strengthening capacity of various cadres of healthcare providers to extend the continuum of care, and providing ongoing mentoring to healthcare providers, can be tested at scale.
This work was supported by Mac Arthur Foundation. The author is grateful to Dr K. G Santhya for her valuable inputs.
Further Reading
- International Institute for Population Sciences (IIPS) and Macro International (2007), ‘National Family Health Survey (NFHS-3), 2005-06: India’, Mumbai.
- IIPS and ICF (2017), ‘National Family Health Survey (NFHS-4), 2015-16: India’, Mumbai.
- Jejeebhoy, SJ and KG Santhya (2014), ‘Sexual and reproductive health: current status and future needs’, in SJ Jejeebhoy, PM Kulkarni, KG Santhya and F Mehrotra (eds.), Population and Reproductive Health in India: An Assessment of the Current Situation and Future needs, Oxford University Press, New Delhi.
- Ministry of Health and Family Welfare (MoHFW) (2005), ‘National Rural Health Mission (2005-2012), Mission Document’, Government of India, New Delhi.
- MoHFW (2013), ‘A Strategic Approach to Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A) in India’, Government of India, New Delhi.
- Paul, Vinod Kumar, Harshpal Singh Sachdev, Dileep Mavalankar, Prema Ramachandran, Mari Jeeva Sankar, Nita Bhandari, Vishnubhatla Sreenivas, Thiagarajan Sundararaman, Dipti Govil, David Osrin and Betty Kirkwood (2011), “Reproductive health, and child health and nutrition in India: Meeting the challenge”, Lancet, 377(9762): 332-49. Available here.
- Paul, S (2018), ‘Are the poor catching up with the rich in utilizing maternal health services? Evidence from India’, Working paper, Population Council, New Delhi.
- Pathak, Praveen Kumar, Abhishek Singh, SV Subramanian (2010), “Economic inequalities in maternal health care: Pre-natal care and skilled birth attendance in India, 1992-2006”, PLoS ONE, 5(10): e13593.




 29 August, 2018
29 August, 2018 




Comments will be held for moderation. Your contact information will not be made public.